A Conversation about Myalgic Encephalomyelitis with Dr. Nina Muirhead

On March 9, 2021, IMHA featured guest speaker Dr. Nina Muirhead for: “A Conversation about Myalgic Encephalomyelitis (ME)”. A medical researcher, surgeon, and educator, Dr. Muirhead was diagnosed with ME in 2017. In this 60-minute webinar, she discusses diagnosis and management of ME, the connection between ME and Long COVID as well as current research.
What is ME?
Myalgic encephalomyelitis (ME), formerly known as chronic fatigue syndrome (CFS) is a devastating, chronic, complex, multi-system disease. Approximately 600,000 individuals suffer from ME in Canada with a female to male ratio of 4:1 (similar to Multiple Sclerosis). It can affect children, adolescents and adults of all ages. Approximately 80% of cases are triggered by a viral infection.
How do we diagnose ME?
There are currently no biomarkers for ME, but a clinical diagnosis can be made using the Canadian Consensus Criteria (CCC). ME patients often present with complaints of crushing exhaustion not relieved by rest, pain or a general sense of feeling unwell that will not go away.
Post-exertional malaise (PEM) is the cardinal feature that separates ME from other causes of fatigue. PEM is often referred to as a “crash”, “flare” or “relapse” and can be triggered by even minimal cognitive or physical exertion. Dr. Muirhead explains, “I thought the person had to do proper exercise like a marathon or a sprint to trigger PEM, when in fact it can be something as simple as brushing your teeth”. Sleep dysfunction, cognitive and neurological symptoms, orthostatic intolerance, Inflammatory Bowel Syndrome (IBS) and/or heart problems, temperature dysregulation, immune system changes, headaches, body and joint pain, light and sound sensitivity are all common symptoms of this debilitating disease.
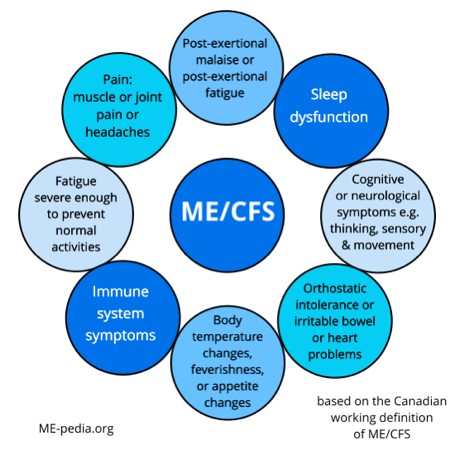
Long description
ME/CFS
- Post-exertional malaise or post-exertional fatigue
- Sleep dysfunction
- Cognitive or neurological symptoms e.g thinking, sensory and movement
- Orthostatic intolerance or irritable bowel or heart problems
- Body temperature changes, feverishness, or appetite changes
- Immune system symptoms
- Fatigue severe enough to prevent normal activities
- Pain: muscle or joint pain or headaches
*based on the Canadian working definition of ME/CFS
Source: ME-pedia.org
What to ask the patient?
Patients typically do not visit their doctor and say, “I've got post-exertional malaise”. Instead, clinicians will hear, “I am still not well” or “I'm having to change what I do”. Questions that might help with a diagnosis are:
- What fraction of your pre-illness capacity are you functioning at?
- What could you do before being ill versus now?
- How many hours a day or a week can you function productively/do useful things?
- How many hours a day are your feet on the floor?
- What happens when you engage in previously tolerated levels of physical or cognitive exertion?
- What can or can't you manage on a good or bad day?
- How long does it take to experience symptoms and to recover (back to baseline) after physical or cognitive effort?
In the webinar, Dr. Muirhead recommended clinicians take a thorough history, make a diagnosis, encourage resting and pacing, check for common co-morbidities like postural orthostatic tachycardia syndrome (POTS), fibromyalgia, IBS and mast cell activation syndrome (MCAS), and manage the symptoms effectively, to improve the quality of life for patients as much as possible. Most importantly, be compassionate and empathetic when meeting patients with ME.
More from Dr. Muirhead: “The current and future research on ME is exciting. We are getting close to finding biomarkers. The global pandemic has brought the world closer—we’re sharing big data, artificial intelligence is growing exponentially, we have improved imaging and neuroimaging, plus more information on epidemiology.“
Summary
- ME is a devastating, chronic, complex, multi-system, heterogeneous disease.
- There is a “crash” or significant flaring of symptoms, called post exertional malaise (PEM), following physical or cognitive exertion. Research has shown that in this illness, exercise and activity-based programs, can make patients much worse, rather than helping.
- The ‘neuroimmune exhaustion’ is pathognomonic of the disease. Severity of symptoms can fluctuate hour to hour, day to day, month to month, year to year.
- Patient harm can occur following failure to recognize and diagnose ME. Wrongly giving advice to do graded exercise therapy or activity-based programs, or even telling the patient to ignore their symptoms (they've often ignored them for far too long by the time they present to the clinician), can be very harmful and can increase their level of severity permanently.
- Support of friends and family, as well as employers, can be very helpful. If patients are school age, their school administrations and teachers should also be informed.
- Early diagnosis, resting/pacing, symptom management and disability support can reduce morbidity.
Thank you Dr. Muirhead and co-host Sabrina Poirier for this important and informative webinar!
Read more: Watch webinar recording
- Date modified: