Community-Based Primary Health Care: Research profiles
Contents
- Introduction
- Innovation teams
- Embedded Clinician Researcher Salary Award
- New Investigator Salary Award
- Applied Public Health Chairs
- Other Researcher profiles
Introduction
The government of Canada launched a CIHR-led Roadmap Signature Initiative to fund research that supports the delivery of high-quality CBPHC across Canada in January 2012. Co-led by the CIHR Institutes of Health Services and Policy Research and Population and Public Health, this Signature Initiative supports researchers to conduct original research on innovative models of care delivery, build capacity for research excellence and translate evidence for uptake into practice and policy. It will achieve this through three major funding tools:
- CBPHC Innovation Team Grants support inter-disciplinary, cross-jurisdictional teams of researchers and decision-makers to conduct excellent research and provide superior research training and mentorship across two key research priorities:
- Access for Vulnerable Populations
- Chronic Disease Prevention and Management
- The Network in Primary and Integrated Health Care Innovations is a key part of Canada’s Strategy for Patient-Oriented Research (SPOR) and the CBPHC Signature Initiative. This SPOR Network will support evidence-informed transformation and delivery of more cost-effective and integrated health care to improve clinical, population health, health equity, and health system outcomes.
- CBPHC Salary Awards
To enable innovation, we need to develop research capacity and leadership for transformative change in community-based primary health care. IPPH and IHSPR are investing in new investigators and applied public health chairs.
This compendium provides profiles of the Innovation Teams and Salary Award recipients funded through the CBPHC Signature Initiative.
Innovation teams
The 12 CBPHC Innovation teams are the most significant investment of the CBPHC Signature Initiative. The Innovation Teams received up to $500,000 per year for up to 5 years. The teams are located throughout Canada and include a range of cross-jurisdictional programs designed to improve access to CBPHC for vulnerable populations and chronic disease prevention and management.
The CBPHC Signature Initiative is made successful through partnerships with a variety of provincial, national and international organizations with a vested interest in supporting improved patient and system outcomes. Key external partners in the CBPHC Innovation Teams competition (2013–2018) include:
- Le Fonds de recherche du Québec – Santé (FRQS)
- Michael Smith Foundation for Health Research
- Australian Primary Health Care Research Institute
- The Health Research Council of New Zealand
Nominated Principal Investigators
-
Marshall Godwin (Memorial University of Newfoundland)
Project title: Atlantic Canada Children’s Effective Service & Strategies in Mental Health (ACCESS-MH)
Principal Investigators: Rick Audas (Memorial University of Newfoundland), Jacques Richard (Université de Moncton), Scott Ronis (University of New Brunswick), Kate Tilleczek (University of Prince Edward Island), Michael Zhang (Saint Mary’s University)
At Issue: Child and youth mental health – Children and youth with mental health and oppositional behavioural problems and their caregivers are among the most vulnerable members of Canadian society. Their conditions are complex and require an interdisciplinary and inter-sectoral approach to provide treatment and care.
Aim: Support improved access to, and experience of, child/youth mental health services in Atlantic Canada
Focus: Five highly prevalent or serious child and youth mental health conditions: Autism Spectrum Disorder (ASD), Conduct Disorder, Eating Disorders, Anxiety and Depression
Jurisdiction: Atlantic Provinces
Approach: We take a broad social sciences approach to each of the these conditions, using Patient Journeys/Process Mapping, Operations Research and Statistical analysis of large and complex databases to develop a comprehensive overview of how children and youth access and experience treatment and services across both the health and education (and potentially other) systems. Best-practice guidelines and a series of tools for service providers will be developed to facilitate better management and outcomes of this vulnerable population.
Team: Our project team includes Primary Health Care Physicians, Policy Makers and Researchers from across Atlantic Canada with the aim to compare the experiences and outcomes of individuals across four different jurisdictions.
Co-Investigators: Bronwyn Davies, Colleen Simms, Roger Chafe, Olga Heath, Don McDonald, William Montelpare, Weiqui Yu, Reid Burke, Julie MacDonald.
Highlights: Created a website, conducted an environmental scan of general mental health services in Atlantic Canada, developed an innovative patient journeys approach to interviewing that incorporates semi-structured interview questions with a visual mapping process and photo-voice elements. A parallel Francophone Patient Journeys project has been established in New Brunswick. Partnered with SEAK (Socially and Emotionally Awards Kids Project) to host the Atlantic Summer Institute on Healthy and Safe Communities symposium Investing in Child and Youth Mental Health – Mobilizing Atlantic Canadians for a Positive Future. The Symposium brought together key stakeholders and decision makers in education, justice and health sectors from across the Atlantic Provinces around the issue of addressing child and youth mental health. Conducted a needs assessment and produced a report for the Autism Society of NL called, REPORT: Needs Assessment Survey Autism Community, Newfoundland and Labrador. The team has produced numerous publications, conferences presentations/posters and various team members have been interviewed.
More Information:
ACCESS-MH
Twitter: @access_MH
ASI 2015 -
Eva Grunfeld (University of Toronto)
Project title: Canadian team to improve community-based cancer care along the continuum (CanIMPACT)
Co-Investigators: Sandy Buchman, Margaret Fitch, Julie Gilbert, Jon Kerner, James Meuser, Carol Sawka, Donna Turner, Fiona Walks, Michèle Aubin, Melissa Brouwers, June Carroll, Craig Earle, Elizabeth Eisenhauer, Lise Fillion, Patte Groome, Ruth Heisey, Amna Husain, Jennifer Jones, Paul Krueger, Monika Krzyzanowska, Aisha Lofters, Donna Manca, John Maxted, Mary McBride, Baukje Miedema, Fiona Miller, Nicole Mittmann, Rahim Moineddin, Mary Ann O’Brien, Geoffrey Porter, Jeffrey Sisler, Jonathan Sussman, Fiona Webster, Marcy Winget
At Issue: Cancer patients rely on good coordination of care between their primary healthcare providers and their cancer specialists throughout their cancer journey from diagnosis to survivorship. However, there are often problems of communication, continuity, and coordination of care that can lead to suboptimal care and anxiety for patients and their families, as well as inefficiency within the healthcare system.
Aim: Tackle the problems of continuity and coordination of care throughout the cancer journey.
Focus: We will focus our research on four specific vulnerable populations (older adults, northern/rural/remote, low income and immigrants) with a special focus on breast cancer.
Jurisdiction: National
Approach: The team is comprehensively studying the factors associated with poor continuity and coordination of care in seven provinces. Second, they will then listen to the perspectives of patients and their families on these aspects of their cancer journey. Third, they will examine the existing medical literature as well as examples of best practices across Canada. Based on what they learn from these steps, they will develop an approach to help healthcare providers, cancer specialists, and patients and their families to work together to improve continuity and coordination of care throughout the cancer journey. At the conclusion of this program of research they will make clear and actionable recommendations on how to improve care for cancer patients and efficiency within the healthcare system.
Highlights: The CanIMPACT Team has developed the CanIMPACT Casebook, which profiles 24 cancer care-specific primary care initiatives across Canada, identifying similarities and differences, strategies used, evaluation, barriers and facilitators and lessons learned. A systematic review (in press) of the peer-reviewed literature was also completed to identify international initiatives and tools to support primary care.
More Information:
The CanIMPACT website
The CanIMPACT Casebook -
Jeannie Haggerty (McGill University)
Project title: Innovative models promoting access-to-care transformation (IMPACT): Supporting the implementation of organisational innovations in community-based primary health care to improve access to care for vulnerable groups
Principal Investigators: Catherine Scott (Alberta Centre for Child, Family and Community Research), Simone Dahrouge (Bruyère Research Institute, CA), Mark Harris (University of New South Wales), Jean-Frédéric Levesque (Bureau of Health Information, AU), Virginia Lewis (Latrobe University, AU), Grant Russell (Monash University, AU), Nigel Stocks (University of Adelaide, AU)
At Issue: Access to care for vulnerable groups – Canada and Australia’s most vulnerable citizens have poor health literacy or are challenged with disproportionately poor access to quality CBPHC although both nations’ champion principles of health equity. Several jurisdictions have implemented changes that aim to enhance the accessibility to, and performance of CBPHC, however, the benefits of these changes are limited as they often do not achieve their objectives in all population groups.
Aim: Design, implement and evaluate local interventions to increase access to PHC for the most vulnerable community members in six participating regions and reduce unnecessary visits to the emergency room and avoidable hospitalisations in each region.
Approach: A five-year program of research using participatory, deliberative processes to design, implement and evaluate organizational innovations that improve access to primary health care for vulnerable populations. The six regional partnerships will have to mobilize the resources to implement the intervention. In return, they are supported by an international team of researchers that focuses on use of data and information to aid them in decisions regarding: access gaps, target populations, components of organisational interventions that can respond to the identified gaps (via the development of a typology of organisational interventions), and contextual implementation of the intervention selected (which is supported by the development of a realist review for each region and intervention); and on evaluating the implemented intervention.
Jurisdiction: Canada (QC, ON, AB) and Australia (NSW, SA, VIC)
Team: An Australian-Canadian collaboration set in six regions (Canada: Quebec, Ontario, Alberta; Australia: New South Wales, South Australia, Victoria), involving local partnerships composed of PHC professionals, decision-makers, researchers and community stakeholders.
Co-Investigators: Mylaine Breton, François Chiocchio, Debbie Feldman, William Hogg, Christine Loignon, Scott Oddie, Pierre Pluye, Kevin Pottie, Shannon Spenceley, Erin Strumpf, Robert Wedel, Vivian Welch, Jenny Advocat, Colette Browning, Benjamin Crabtree, John Glover, Jane Gunn, Terry Haines , Anthony Harris, Paul Jennings, Riki Lane, Siaw-Teng Liaw, Donna Markham, Julie Mc Donald, Lisa McKenna, William Miller, Stephen Peckham, Gawaine Powell Davies, Martin Roland, Nicolas Senn, Ann Taylor, Nicholas Zwar, Denis A. Roy, Danièle Francoeur, Stephen Christley, Antoine Groulx, Lisa Halma, Jean Rodrigue, Shelly Park, Rene Pennock, Anne Peek
Highlights: The IMPACT team has developed a common evaluation framework for 6 different interventions. The goal is to support comparisons of results within and across countries.
From the beginning IMPACT focused on the partnership development to fund intervention to be implemented locally. This was high risk venture that paid off.
More Information: IMPACT
-
Stewart Harris (University of Western Ontario)
Project title: Transformation of Indigenous Primary Healthcare Delivery (Forge Ahead): Community-Driven Innovations and Scale-Up Toolkits Stewart Harris
At Issue: Chronic disease management services in First Nations communities: Given the dramatic rise and impact of chronic disease in Indigenous Peoples in Canada, a shift from the existing health care model commonly employed in First Nations communities, to one that integrates prevention and chronic disease management is required.
Focus: Type 2 diabetes mellitus.
Jurisdiction: 11 First Nations communities in 6 provinces across Canada.
Aim: Develop and evaluate community-driven, culturally relevant, primary healthcare models that enhance chronic disease management and appropriate access to available services in First Nations communities in Canada.
Approach: A series of 10 inter-related and progressive projects that will foster community-driven initiatives with type 2 diabetes mellitus as the action disease. FORGE AHEAD will use a participatory research approach that simultaneously ensures culturally appropriate implementation and integrates knowledge translation by involving relevant stakeholders throughout the entire program.
Program overview
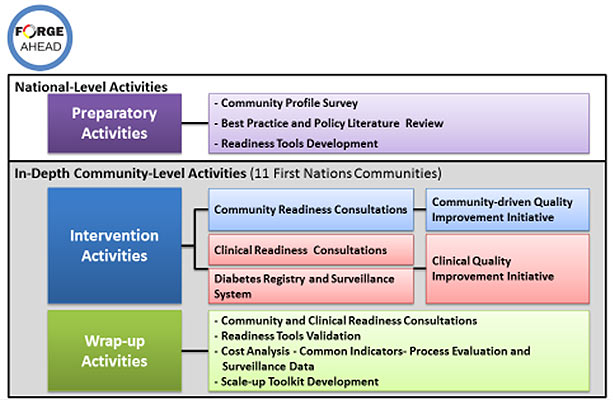
Project title: FORGE AHEAD - Program Activities Overview - Long Description
National level activities
Preparatory Activities
- Community Profile Survey – all 617 First Nations Communities
- Best Practice and Policy Literature Review
- Readiness Tools Development
In-depth Community-level Activities (~14 First Nations Communities)
Intervention Activities
- Community Readiness Consultations - Community-driven Quality Improvement Initiative
- Clinical Readiness Consultations - Clinical Quality Improvement Initiative
- Diabetes Registry and Surveillance System - Clinical Quality Improvement Initiative
Wrap-Up Activities
- Community and Clinical Readiness Consultations
- Readiness Tools Validation
- Cost Analysis - Common Indicators- Process Evaluation and Surveillance Data
- Scale-up Tool Kit Development
Team: The multi-disciplinary and cross-jurisdictional research team includes First Nations community representatives, Indigenous and non-Indigenous healthcare providers, clinician scientists, academic researchers reflecting a wide variety of disciplines from across Canada and policy decision-makers.
Co-Investigators: Ed Barre, Onil Bhattacharrya, David Dannenbaum, Keith Dawson, Roland Dyck, Jo-Ann Episkenew (in memory), Michael Green, Anthony Hanley, Barry Lavallee, Ann Macaulay, Alex McComber, Monica Parry, Sonja Reichert, Jonathan Salsberg, Amardeep Thind, Sheldon Tobe, Ellen Toth, Audrey Walsh, Lloy Wylie, Merrick Zwaranstein, Heather McDonald, and Braden Te Hiwi.
Highlights: The FORGE AHEAD Team has implemented community-level quality improvement intervention activities with 11 First Nations communities partnered in the program. These activities are aimed at generating stakeholder-driven community and clinical quality improvement initiatives in diabetes prevention and management. Clinical team members have used quality improvement tools and resources to try out small tests of change, through the PDSA cycles, in primary care delivery – these are on-the-ground innovations to improve appointment attendance, communication across the clinical team, patient follow-up, use registry and surveillance data to enhance patient-centered visits, and the overall patient experience. Additionally, community team members, also through the PDSA cycles, have mobilized and leveraged resources to establish interventions to increase physical activities, improve awareness about diabetes and diabetes programs and services, undertake educational activities around nutrition and healthy eating, and establish relationships with other community-based groups to improve care and coordination.
More Information:
Website. Our website contains current information on the FORGE AHEAD Research Program including links to the Program Description, Program Timeline, News & Events, and Newsletters.
Program Coordinator: Harsh Zaran
E: harsh.zaran@schulich.uwo.caGeneral Inquiries: E: forgeahead@schulich.uwo.ca
T (toll-free): 1-855-858-6872
F (toll-free): 1-877-809-5108 -
Janusz Kaczorowski (Université du Montréal)
Project title: Canadian chronic disease awareness and management program (C-ChAMP)
Principal Investigators: Tamara Daly (York University), Lisa Dolovich (McMaster University), Marie-Thérèse Lussier (Université du Montréal), Simone Dahrouge (University of Ottawa)
At Issue: Chronic disease prevention and management - The most prevalent chronic health conditions are largely the product of interactions among a small set of well-established, modifiable risk factors that include smoking, sedentary lifestyle, heavy alcohol drinking and high salt consumption. These risk factors are in turn responsible for rise nationally and internationally in chronic health conditions, notably diabetes and cardivascular diseases.
Aim: To improve community and population-based prevention and management of chronic disease.
Focus: Cardiovascular health among younger participants, ethnic minority populations (South-Asians), and populations in large urban and suburban communities.
Jurisdiction: Ontario and Quebec
Approach: Based on the success of the Cardiovascular Health Awareness Program (CHAP), C-ChAMP will engage the multi-disciplinary and inter-sectoral team in adapting the program to different populations and settings, and work toward identifying the optimal conditions for the program’s sustainability and scalability.
Team: Social scientists, pharmacists, family physicians, nurses, specialists, epidemiologists, biostatisticians, health economists, decision makers, patients, and others for our research team.
Co-Investigators: Angelique Berg, Martine Montigny, Vasanthi Srinivasan, Sheldon Tobe, Farah Ahmad, Ricardo Angeles, Maria Chiu, Alexandra Fletcher, Ron Goeree, Johanne Goudreau, Charlotte Jones, Lyne Lalonde, Beatrice Mcdonough, Véronique Grenier, Michael Paterson, Jane South, Iffath Syed, Jean-Claude Tardif, Lehana Thabane, Karen Tu, Gina Agarwal, Danielle Wolfe.
Highlights: CHAP was originally developed for seniors living in small to medium-sized communities. Current work has expanded its reach to younger adults (Laval in Quebec and Markham in Ontario), ethnic communities (South-Asian population in Markham, Ontario), older adults living in subsidized housing (Hamilton, Ontario), and individuals in large urban and suburban communities in Alberta, Ontario and Quebec. They are also offered in a variety of new settings including Family Health Teams, subsidized housing, community centres, schools, libraries and places of worship. Sessions now include prediabetes, type 2 diabetes and mental health awareness and screenings, and detection of atrial fibrillation. Volunteer recruitment and training methods have been adapted to meet the needs of CHAP communities and target populations. Sessions are facilitated by age-matched locally recruited volunteers (Laval, Quebec), university students (Markham and Ottawa, Ontario) or paramedics (Hamilton, Ontario).
The CHAP has been expanding beyond the scope of the CBPHC team grant. In the past two years only, the program has attracted over $11M in additional research funding to adapt, implement and evaluate the CHAP for, among others, older adults living in subsidized housing in Hamilton (Ontario), in community pharmacies in Ontario and Alberta (C-SPIN), and more recently in one of the poorest regions of the Philippines, as a first step in targeting other populations in low-and-middle income countries. The team is also working on ways to adapt and extend CHAP to other Low and Middle Income Countries (LMICs) and has established an advisory committee with members from Nepal, Thailand and Tunisia.
Figure 1: Evolution of CHAP into C-ChAMP
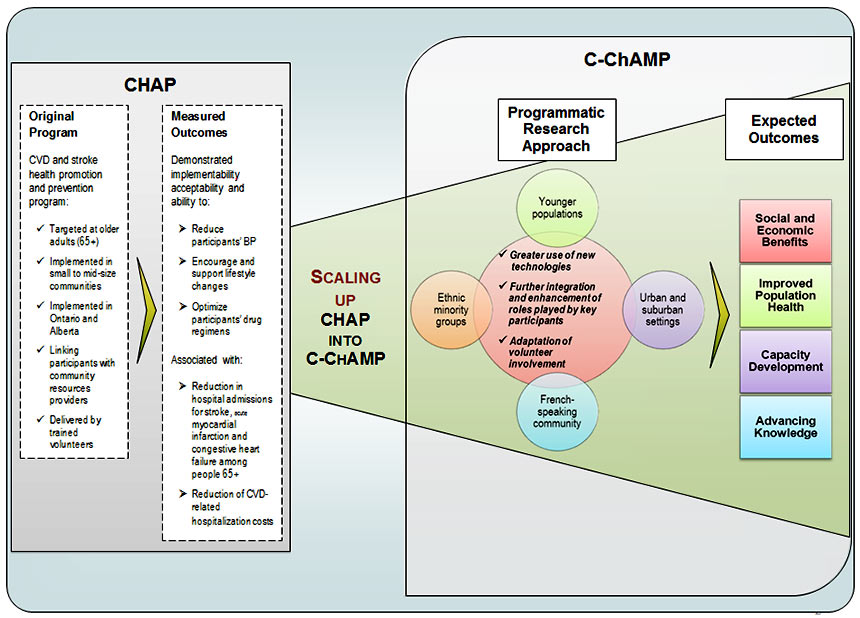
Figure 1: Evolution of CHAP into C-ChAMP - Long Description
CHAP
Original Program
CVD and stroke health promotion and prevention program:
- Targeted at older adults (65+)
- Implemented in small to mid-size communities
- Implemented in Ontario and Alberta
- Linking participants with community resources providers
- Delivered by trained volunteers
Mesured Outcomes
Demonstrated implementability acceptability and ability to:
- Reduce participants' BP
- Encourage and support lifestyle changes
- Optimize participants' drug regimes
Associated with:
- Reduction in hospital admissions for stroke, acute myocardial infarction and congestive heart failure among people 65+
- Reduction of CVD-related hospitalization costs
Scaling up CHAP into C-ChAMP
C-ChAMP
Expected Outcomes Programmatic Research Approach Social and Economic Benefits Ethnic minority groups - Greater use of new technologies
- Further integration and enhancement of roles played by key participants
- Adapatation of volunteer involvement
Improved Population Health Younger populations Capacity Development Urban and suburban settings Advancing Knowledge French-speaking community -
Alan Katz (University of Manitoba)
Project title: Innovation in community based primary healthcare supporting transformation in the health of First Nations and rural/remote Manitoba communities: iPHIT
Principal Investigators: Kathi Avery Kinew (Assembly of Manitoba Chiefs), David M Greggory (University of Regina), Josée G Lavoie (University of Manitoba)
At Issue: Primary healthcare transformation in rural and remote First Nations communities – the poor health status and higher rates of hospitalization experienced by many First Nations is evidence of the need to invest in effective CBPHC. Evidence suggests that beyond their isolated locations and often disadvantaged socio-economic status, First Nations and rural and remote communities inherit policy decisions made with urban centres in mind, which may contribute to negative health outcomes.
Aim: Explore the community understanding of primary care and identify effective CBPHC models in FN communities in order to enable the development and implementation of health care models to improve the scope and delivery of CBPHC services and bring about better health outcomes.
Jurisdiction: 8 rural and remote Manitoba First Nations
Approach: Engagement with participating communities to understand the current state of CBPHC in First Nations and rural and remote Manitoba, understand local perspectives on their health and needs and propose innovative local models of care that can improve the health of the communities. Local Research Assistants hired and trained locally to support the implementation of the program of research within in each participating community. The final stage will include an evaluation of the implementation of some of these new models of care.
Team: The iPHIT grant has facilitated the building of a strong working relationship between academic primary care researchers and a dynamic team of collaborators. These include the Assembly of Manitoba Chiefs (AMC), and Nanaandewewigimig, First Nation Health and Social Secretariat of Manitoba (established by the AMC in 2014), the MFN Centre for Aboriginal Health Research, and 8 First Nations communities.
Co-Investigators: Norman Bone, Valerie Gideon, Avis Gray, Marcia Anderson, Melanie MacKinnon, Stephanie Sinclair, Leona Star.
Highlights: Team Members based in each of the 8 First Nations communities involved in the iPHIT initiative have recruited and trained Local Research Assistants (LRA). The LRA’s have conducted qualitative interviews for the first phase of the program of research; administered surveys for the Common Indicator project and organized community feedback and validation workshops in their respective communities. Our analyses of administrative data have resulted in intriguing findings with regard to ambulatory care sensitive hospitalizations over time across different primary care service models in First Nations Communities.
Next steps: Primary care transformation in First Nations communities needs to be based on local circumstances, values and culture. Each of the 8 communities have unique needs (as do urban environments) which will require community specific plans for transformation.
-
Claire Kendall (University of Ottawa), Clare Liddy (2013-16) (Bruyère Research Institute, University of Ottawa)
Project title: Advancing primary healthcare for persons living with HIV in Canada
Principal Investigators: Shabnam Asghari (Memorial University of Newfoundland), Marissa Becker (University of Manitoba), Christopher P. Kaposy (Memorial University of Newfoundland, 2013 - 2016), Sean B. Rourke (Ontario HIV Treatment Network)
Principal Knowledge Users: Carla Loeppky (Government of Manitoba), Frank McGee (Ontario Ministry of Health and Long Term Care)
At Issue: Thanks to improvements in care and treatment strategies, people with HIV are living longer and have a better quality of life. These advances have brought new challenges. HIV has evolved from an acute to a chronic condition characterized by multiple co-morbidities. Diseases of aging such as diabetes, cardiovascular disease, and cancer are now common among this population group. Given this evolution, the way that HIV care is organized and delivered in Canada may no longer meet the needs of its target population.
Aim: To conduct the foundational work required to shift the majority of HIV care to the community-based primary health care (CBPHC) community, while maintaining essential ties to specialist HIV care. Our research and interventions will help us improve the primary health care sector’s capacity to provide comprehensive, integrated HIV care.
Jurisdictions: Manitoba, Ontario, Newfoundland & Labrador.
Approach: We will close gaps in the continuum of care for people with HIV by developing quality of care indicators, introducing eHealth solutions to support physician decision-making, create decision support guidelines, tool-kits and self-management protocols to enable patients and providers to better navigate the HIV continuum of care. Our academic-policy-provider-community partnerships will help us move the knowledge we create into action and enhance the impact of our knowledge translation strategy. These partnerships will facilitate dissemination of evidence to stakeholders across all sectors and help us transform the capacity of the primary care sector to provide comprehensive, integrated HIV care.
Co-Investigators: Jill Allison, Tony Antoniou, Gordon Arbess, Jean Bacon, Ahmed Bayoumi, Christine Bibeau, Ann Burchell, Kimberley Burt, Tara Carnochan, Timothy Christie, Kayla Collins, Gerard Farrell, Richard Glazier, Dale Guenter, Jennifer Gunning, William Hogg, Laurie Ireland, Sharon Johnson, Erin Keely, Deborah Kelly, Jelani Kerr, Cynthia Kitson, Colin Kovacks, Mona Loufty, Philip Lundrigan, Douglas Manuel, Meaghan McLaren, Leonard Moore, Gerry Mugford, Elizabeth Muggah, Andrew Pinto, Kevin Pottie, Anita Rachlis, Robert Remis, Timothy Rogers, Ron Rosenes, Cheryl Schultz, Tina Sorensen, Monica Taljaard, Kednapa Thavorn, Mark Tyndall, Nancy Yu.
Highlights: The LHIV Innovation Team is on target with our proposed timelines, with some projects completed and multiple projects underway. Completed projects include the development of a performance framework, measures (i.e. indicators) of community-based care for people living with HIV/AIDS (PLHA), and a scoping review of HIV patient perspectives on access to care. The cohort development work has been completed across all three participating provinces (MB, NL, ON) and the comprehensive cohort analysis is underway, which will allow our team to use real data from the administrative cohorts to characterize the treatment cascade in order to drive interventions. Examples of completed administrative analyses include identification of gaps in end-of-life care, cancer screening, and linkage to care after diagnosis. We have completed a cross-Canada survey of clinics providing care to PLHA, and are undertaking key informant interviews to better understand the survey results (focusing on aspects of the patient-centred medical home). Patient surveys are underway using the Patient Activation Measure©. An institutional ethnography study in NL and MB is complete, exploring ethical issues in providing care to PLHA, and results will be published soon. Multiple projects in understanding self-management supports for PLHA are in the conceptual stage, with implementation planned for Years 4 and 5.
At the CBPHC meeting in October 2016, we will be highlighting the success of the Champlain BASE™ (Building Access to Specialists through eConsultation) eConsult service. The goal of this service is to provide faster access to specialty care for Canadians, using eConsultation to improve intraprofessional communication. It has proven to be highly successful and been implemented in two health regions in Ontario, with a launch of a pilot project in NL expected in the fall of 2016. Through its national partnerships, including connections made through this CBPHC collaboration, several health regions/provinces are interested in implementing similar services using this proven model of care, including BC, AB, NT, MB, ON, QC, NS and NL. The Champlain BASE™ eConsult service has become a world leader in eConsultation and continues to promote this model of care that is novel, effective, efficient and low-cost—a much needed health services innovation.
More Information:
-
Walter Wodchis (University of Toronto)
Project title: Implementing models of primary health care for older adults with complex needs
Principal Investigators: Tim Kenealy (University of Auckland), Mylaine Breton (U Sherbrooke)
Principal Knowledge Users: Fredrika Scarth (Ontario MOHLTC), Karen Evison (NZ DOH)
Focus: Approaches to scaling-up successful interventions – Most countries are seeking knowledge of better models of CBPHC delivery to address emerging challenges to manage chronic disease and to improve the value of the health system. People need a health system that addresses their needs, either minor and discrete or complex and continuous. Decision makers in the health system need to understand what they can do to facilitate innovation that results in better care, improved population health, and cost management. Clinicians need more collaborative models of care delivery that facilitate patient-centred care particularly for individuals with complex needs.
Aim: The goal of the research program is to understand how to scale-up successful innovative models of CBPHC. A population-based model that improves access and quality of occasional contacts for most and intensive well-managed care for individuals with complex care needs and high cost is needed to achieve better care, improved health, and cost management.
Approach: We will implement a three-phase program of research based in Canada and New Zealand wherein we will discover, develop and compare innovative delivery models of CBPHC and assess the contextual conditions associated with success or failure.
Jurisdiction: Quebec, Ontario and New Zealand
Co-Investigators: Melissa Farrell, James Meloche, Geoffrey Anderson, Ross Baker, Janet Barnsley, Peter Carswell, Martin Connolly, Yves Couturier, Jean-Louis Denis, Janet Durbin, Dominique Gagnon, Tim Kenealy, Anna Koné Péfoyo, Kerry Kuluski, Fiona Miller, John Parsons, Nicolette Sheridan, Ross Upshur, Paul Williams.
Highlights: The iCOACH Team (Implementing Integrated Care for Older Adults with Complex Heath) has engaged and worked closely with decision makers from the outset of the initiative, which aims to understand how to scale-up successful innovative models of CBPHC. The team has already been able to share preliminary findings and recommendations with key health systems stakeholders – Directors, Assistant Deputy Ministers and the Deputy Minister. We are now planning an application of our knowledge in the spread of a province-wide integrated care initiative in Ontario. We have a forthcoming special issue of the International Journal of Integrated Care late fall 2016 with 10 manuscripts from the team.
-
Moira Stewart (University of Western Ontario)
Project title: Patient-centred innovations for persons with multimorbidity (PACE in MM)
Principal Investigators: Martin Fortin (Université du Sherbrooke)
At Issue: Patient-centred chronic disease prevention and management – Males and females with chronic conditions are likely to have more than one condition, but the health care system is mostly designed for managing one condition at a time.
Aim: Our team proposes innovations in chronic disease prevention and management (CDPM) that will: reorient care from a single disease focus to a multimorbidity focus; centre on not only disease but also the patient in context; and realign the health care system from separate silos to coordinated collaborations.
Approach: The research will analyse female and male patients separately in three parts of the proposed research: first when examining existing initiatives for Chronic Disease Prevention and Management in a Realist Synthesis; second in a qualitative study of innovations; and third when testing the innovations in care in relation to outcomes of patient health and the health care system. Patients’ gender characteristics will be analysed during the testing of the innovations in care through examining patients’ perspectives of professional or working status, marital and family status, social engagement, and gender identity. We anticipate impacts on important patient intermediate self-perceived outcomes (empowerment and self-management, psychological distress, self-efficacy in managing chronic disease, quality of life) as well as health services utilization and cost.
Jurisdiction: Ontario, Quebec, British Columbia, Manitoba, Nova Scotia, New-Brunswick
Co-Investigators: Martine Couture, Paul Huras, Onil Bhattacharyya, Judith Brown, Maud-Christine Chouinard, Frances Gallagher, Richard Glazier, William Hogg, Alan Katz, Christine Loignon, Jonathan Sussman, Amardeep Thind, Walter Wodchis, Sabrina Wong, Merrick Zwarenstein, Valérie Emond, Tara Sampalli, Sonja Reichert, Roxanne Borges Da Silva, Helena Piccinini-Vallis, Mathieu Belanger, [To be confirmed: Jocelyn Charles, Pauline Pariser, Thuynga Pham].
Highlights: The PACE in MM Team conducted an Environment Scan and Realist Synthesis of CPDM initiatives linked to the primary care reform to identify factors responsible for their success or failure. As a result of this work the team has produced a Chronic Disease Prevention and Management toolkit that has been presented to different audiences in 3 provinces.
Through engagement of key stakeholders and decision makers on their team, the PACE in MM Team was also able to distill all the information gathered and decide upon one program to evaluate in Quebec and one in Ontario. Both Quebec and Ontario have health care systems that have been shaped and guided by different histories, priorities, political experiences, fiscal realities and current focus of each government. The interventions that were ultimately selected have arisen out of the real world of practice and policy and address the needs each government to find better CDPM programs. While each program is different, they will be able to evaluate and compare common outcome measures and help facilitate evidence-based scale up.
In Ontario, the team will evaluate the Telemedicine Impact Plus program – a program based on patient-centred care and that targets the most complex patients. It provides coordinated care by facilitating an interdisciplinary team including the patient via teleconference, helping to increase care outcomes and reduce unnecessary ER visits.
In Quebec, the PACE in MM team will evaluate Démarche intégrée de prevention et gestion des maladies chroniques – Région 02 (DIMAC02), a program which aims to make available, in Family Medical Groups, a patient-centred interdisciplinary educational intervention targeting multiple chronic diseases. The program also aims to increase the flow of communications between Family Medical Groups and actors of the healthcare system regionally to improve continuity of care.
According to Martine Couture, Présidente-Directrice Générale du Centre Intégré Universitaire de Santé et de Services Sociaux du Saguenay−Lac-St-Jean, the PACE in MM research program “…has ensured that Quebec innovations have been enhanced and scaled-up to the whole Saguenay region, a major impact. The research team has involved me in the entire process, from proposal writing to implementation and evaluation.”
More Information: PACE in MM
-
Jenny Ploeg (McMaster University)
Project title: Innovative community-based approaches to promote optimal aging for older adults with multiple chronic conditions and their caregivers
Principal Investigators: Kaiyan Fu (Ontario Ministry of Health and Long-Term Care), Anne Hayes (Ontario Ministry of Health and Long-Term Care), Maureen Frances Markle-Reid (McMaster)
At Issue: Optimal aging at home – Given the unprecedented aging of the population, older adults with two or more Multiple Chronic Conditions (MCC) are a public health priority. People with MCC account for 40 per cent of reported health care use among seniors in Canada, and the intensity of health care use increases as the number of chronic conditions increases. MCC can impair clients’ ability for self-management and adherence to treatment, which increases the probability of adverse health outcomes.
Aim: The aim of the Aging Community and Health Research Unit (ACHRU) is to design, implement, evaluate and translate new integrated and person-centered interventions that enhance patient and caregiver outcomes, and reduce costs, to promote optimal aging at home.
Jurisdiction: Alberta and Ontario
Approach: Conducting six interrelated studies, in Alberta and Ontario, which focus on the prevention and management of MCC in community-living older adults and support family caregivers. The research objectives are: 1) to understand how older adults with MCC, family caregivers and health professionals manage MCC; 2) to examine the factors, health outcomes and costs associated with MCC; 3) to examine the feasibility and acceptability of multi-component interventions to promote health and/or self-management of chronic conditions, such as interdisciplinary teams, peer support, navigators, and mobile or internet-based support; and 4) to determine the effectiveness of the interventions on client and caregiver outcomes and costs.
Team: This pan-Canadian CIHR-funded program is conducted by an interdisciplinary team of investigators, health professional scientists and clinicians who, in turn, are advised by stakeholders including patients and families, and senior health system decision-makers. The program includes an active capacity building strategy led by trainees.
Co-Investigators: Carol Anderson, Melissa Farrell, Susan Paetkau, Noori Akhtar-Danesh, Susan Baptiste, Duane Bender, Wendy Duggleby, Anna-Marie Emili, Sid Feldman, Dorothy Forbes, Kimberly Fraser, Amiram Gafni, Rebecca Ganann, Anna Garnett, Sunita Ghosh, Margaret Gibson, Lauren Griffith, Andrea Grunier, Sandra Hirst, Sharon Kaasalainen, Janice Keefe, Nancy Matthew-Maich, Carrie McAiney, Christopher Patterson, Shelley Peacock, Carlos Rojas-Fernandez, Cheryl Sadowski, Jean Triscott, Ross Upshur, Ruta Valaitis, Allison Williams.
Highlights: Three interventions are currently being evaluated in pragmatic, multi-site randomized control trials in Alberta and Ontario. They include trials of an online transition toolkit for family caregivers of persons with MCC and dementia, a community partnership program for community living older adults with MCC and Type 2 Diabetes Mellitus, and a community partnership program for older adults with MCC and vascular conditions using home care services (Ontario only).
More Information: Aging, Community and Health Research Unit
-
Sabrina Wong (University of British Columbia)
Project title: Transforming CBPHC delivery through comprehensive performance measurement and reporting
Principal Investigators: Bill Hogg (Bruyère Research Institute), Fred Burge (Dalhousie University)
At Issue: Comprehensive performance measurement and reporting for improved quality of care – A strong community-based PHC (CBPHC) system will give Canadians more equitable care with better population outcomes at reduced cost. Canada has made substantial financial investments in renewing CBPHC over the last decade. Yet, no information system exists to routinely capture whether renewal efforts improve CBPHC performance or quality of care in Canada.
Aim: Improve the science and reporting of CBPHC performance in order to demonstrate the feasibility and usefulness of comparative CBPHC performance measurement, reporting at a jurisdictional level that can inform future innovation in the delivery and organization of PHC services.
Approach: Conduct 4 interrelated studies in order to compare measures of CBPHC performance and healthcare equity between regions, including comparative performance for complex vulnerable patients; examine contextual factors that may explain regional variation; develop and evaluate an approach to national reporting of CBPHC performance based on priorities and optimal reporting formats; identify innovations of service delivery associated with better CBPHC performance and healthcare equity; examining cost effective technology solutions to further develop a CBPHC information system and create real-world problem-solving ability in a learning community.
Jurisdiction: British Columbia, Ontario, Nova Scotia
Co-investigators: Julia Abelson, Medhi Ammi, Mary Byrnes, John Campbell, Heather Davidson, Khaled El-Emam, Rick Gibson, Richard Glazier, Anna Greenberg, Jeannie Haggerty, Sharon Johnston, Alan Katz, Victoria Lee, Jacques Lemelin, Ruth Martin-Misener, Kim McGrail, Paul Roumeliotis, Tara Sampalli, Claudia SanMartin, Cathie Scott, Walter Wodchis
Collaborators: Annette Browne, Phil Emberley, Marilyn Ford-Gilboe, Bev Holmes, Anthony Mar, Monica Taljaard, Colleen Varcoe
Highlights: To date, the TRANSFORMATION Team has collected patient reported experiences, impacts and outcomes from 2000+ primary care patients in Central Zone, Nova Scotia, Eastern Ontario, Ontario and Fraser East, British Columbia; engaged primary care patients through deliberative dialogues in these three sites; and completed a policy document review assessing their guidance for innovations in CBPHC. They have built active International and regional advisory stakeholder committees, engaged in local performance measurement initiatives across Canada, and built team and trainee capacity in using relevant research methods and tools. They have collaborated on developing a social vulnerability index which will be used to report on healthcare equity. Their work suggests segmenting populations to monitor performance across different domains of PHC is important. The TRANSFORMATION Team has also piloted an automated survey system for collecting patient experience data – a cost-effective and innovative ‘first’ in Canada. Further piloting has evolved in other jurisdictions and new collaborations with a software company have emerged from this work.
More Information: Twitter: @transformphc
-
Kue Young (University of Alberta)
Project title: Transforming primary healthcare in remote northern communities: The circumpolar health system innovation team [CIRCHSIT]
Principal Investigators: Michael Jong (Labrador–Grenfell Regional Health Authority), James D Ford (McGill University), Josée G Lavoie (University of Manitoba, Centre for Aboriginal Health Research), Arto E Ohinmaa (University of Alberta), Mason White (University of Toronto)
At Issue: Remote northern health – Health care in Canada’s North faces considerable challenges with its remote and widely dispersed population, harsh environmental conditions, and thinly deployed health professionals. Despite per capita expenditures that are among the highest in the world, health outcomes continue to lag behind the rest of Canada, and health disparities between the Aboriginal and non-aboriginal population within the North continue to persist.
Aim: The Circumpolar Health System Innovation Team [CircHSIT] is designed to provide research evidence to enable the transformation of PHC in remote northern communities in Canada, through the design, implementation, and evaluation of health systems interventions and technology innovations.
Jurisdiction: Northwest Territories, Nunavut and Labrador. Other circumpolar regions (Alaska, Greenland, Nordic countries and Russia) will be covered in comparative policy and statistical reviews but not field work.
Approach: CircHSIT stresses developing community capacity to contribute to and fully participate in health system improvements and collaborating with decision makers to ensure rapid translation and application of research outputs. CircHSIT consists of three core components: Part One explores policy options in PHC and assesses health systems performance across circumpolar regions. Part Two develops innovations at different points along the patients’ pathway to care, at the pre-encounter, encounter, and post-encounter phases. Projects investigate medical emergencies out on the land away from professional help, alternative models of health care architecture, a territory-wide chronic disease registry for monitoring clinical care, the use of remote presence technology in chronic disease management, frontline providers’ perspectives on medevac decision making, and rationalizing the referral and transfer systems from communities to regional hospitals. Part Three is capacity building, especially the development of northern-based research centres and mentorship of northern-based faculty.
Co-Applicants: Ewan Affleck, Adalsteinn Brown, Susan Chatwood, Gwen Healey
Highlights: The CircHSIT Team has been successful in establishing a new StatsCan Research Data Centre in Yellowknife – the first such centre to be housed outside of a university. This has established access to pooled datasets from a variety of national surveys and enabled the team to examine health care access and other issues in the North disaggregated by region and ethnicity.
In April 2016 the team organized an international conference on Transforming Health Care in Remote Communities with 150 participants from academe, governments, health care agencies, community organizations and the private sector from 7 countries. It provided an opportunity to present their mid-term findings and also meet new potential partners with similar interests. The conference was opened by the Minister of Health of the Northwest Territories and also heard from presentations from the deputy health ministers from both NWT and Nunavut.
Embedded Clinician Researcher Salary Award
The Embedded Clinician Researcher Salary Award program is led by the CIHR Community Based Primary Health Care Signature Initiative (CBPHC) and the CIHR Institute of Health Services and Policy Research (IHSPR), in partnership with the following CIHR institutes:
- CIHR Institute of Indigenous Peoples' Health (IIPH)
- CIHR Institute of Cardiovascular and Respiratory Health (ICRH)
- CIHR Institute of Musculoskeletal Health and Arthritis (IMHA)
- CIHR Institute of Nutrition, Metabolism and Diabetes (INMD)
- CIHR Strategy for Patient Oriented Research (SPOR)
As well as with the following external partners:
- Health Quality Ontario (HQO)
- New Brunswick Health Research Foundation (NBHRF)
This salary award program is designed to build capacity for, and support the creation of, Learning Health Systems – accountable healthcare organizations that mobilize research for transformation and impact, particularly to improve patient experience and outcomes, and quality of life for persons with chronic conditions.
There were 20 Embedded Clinician Researcher Salary Award recipients funded, receiving $75,000 per year for up to 4 years. The award is offered to early- to mid-career health services and policy researchers holding active licensure as a health professional that are clinicians first but need protected time to engage in research that is critical to advancing change. Applicants were required to secure partner contribution(s), including at least one from a health system partner organization, of $25,000 (cash) per annum towards salary costs over four years and $50,000 (cash or in-kind) per annum towards research costs over four years.
Nominated Principal Investigators
-
Dr. Keith Ahamad, University of British Columbia

Project title: Engaging primary care through research and education as the key to improving access to evidence-based addiction treatment in Canada
Embedded Health System Partner: BC Centre for Excellence in HIV/AIDS
Brief Bio: After a 7-year career in computer engineering, Dr. Keith Ahamad returned to school to become a doctor in 2003 inspired after volunteering at a community clinic needle exchange. He completed his Medical Degree at UBC in 2010 and his residency in Family Medicine at UBC and subsequently trained in addiction medicine. Today, he works as an addictions physician at St. Paul’s Hospital and a researcher with Dr. Evan Wood at the BC Centre for Excellence in HIV/AIDS. He has focused his work and research on addiction medicine, attending to patients with a range of drug addictions and other health challenges.
At Issue: Untreated alcohol and drug addiction is linked to an enormous burden of disease. Bringing evidence into prevention, treatment, and care for substance use disorders is key to managing the huge health and social costs of untreated alcohol and drug addiction. Strategies to incorporate evidence into addiction care include the development of clinical guidelines and other tools of practice, and filling the gaps in clinical education, particularly in primary care.
Aim: There is also a need for individual components of the addiction care system to connect, rather than operate independently of one another, to improve patient access to treatment across all aspects of care. The program of research aims to shift this by advancing evidence-based addiction care and treatment through primary care.
Focus: Our health care system is currently not equipped to recognize, prevent, diagnose and treat substance use disorders in an evidence-based way. The majority of addiction care is provided in specialty clinics with very long wait times and historically poor outcomes. Improving access to evidence-based addiction care is essential to reduce the burden of this disease. Primary care is ideal and critical for the response due to the chronic relapsing nature of addiction and the longitudinal, ubiquitous on-demand nature of primary care.
Jurisdiction: Provincial (BC)
Approach: The program of research will actively engage health care providers, researchers, and allied health professionals in the advancement of evidence-based addiction care and treatment. The program intends to close the research to practice gap by developing and implementing evidence-based guidelines, creating and evaluating care pathways that target gaps in the health care systems, strengthening evidence by conducting a robust program of clinical trials, and mentoring and training the next generation of health care professionals in evidence-based addiction medicine and clinical research.
Team: University of British Columbia and the BC Centre for Excellence in HIV/AIDS
-
Dr. Patrick Archambault, Université Laval

Project title: Supporting the creation of a learning integrated health system to mobilize context-adapted knowledge with a wiki platform to improve the transitions of frail seniors from emergency departments to the community: The learning wisdom program
Embedded Health System Partner: Centre intégré de santé et de services sociaux de ChaudièreAppalaches
Brief Bio: Dr. Patrick Archambault obtained his medical degree from Université Laval in 2000 and completed his post-graduate training to become a member of the Royal College of Physicians and Surgeons of Canada as an emergency medicine specialist at Université Laval in 2005. He was awarded the McLaughlin Fellowship bursary by the Dean of the Faculty of Medicine at Université Laval and, in 2007, completed a Royal College subspecialization in critical care medicine in Ottawa. Dr. Archambault graduated with honours from the Master’s program in clinical research at Université Laval in 2007 and the Royal College awarded him a Certificate of Completion in the clinician investigator program. During his Master's studies, Dr. Archambault studied the negative impact of etomidate on the production of cortisol in traumatic brain injuries. Between 2008 and 2010, he completed a CHSRF-funded research fellowship under the co-direction of André Lavoie, Jean Lapointe and France Légaré (Canada Research Chair for Shared Decision Making and Knowledge Translation). Since January 2008, he has been working in the Emergency Department and the Intensive Care Unit of the Hôtel-Dieu de Lévis. In 2012, he was awarded a Junior 1 FRQS clinician-scientist award to lead a KT research program exploring the use of a wiki platform to support the implementation of best practices in the field of trauma care. His research has been conducted with the support and mentorship from KT Canada and the Canadian Critical Care Trials Group. He is currently co-leading the knowledge translation function within the Réseau-1 Québec FRQS knowledge network in integrated primary care and services.
At Issue: Elderly patients discharged from emergency departments are often repeatedly readmitted, lose functioning capacity, and increase caregivers' burden of care. Care becomes fragmented, discontinuous, and costly. In addition, Quebec's Bill 10 has merged healthcare institutions but has not yet integrated their information, human resources or care management systems, resulting in further fragmentation of care. However, using proven (evidence-based) strategies can improve transition for the elderly. The Acute Care for Elders Program at Mount Sinai applied innovative strategies (interventions) which reduced lengths of hospital stay, reduced readmissions, increased patient satisfaction, and saved over $6 million in 2014. Strategies included providing transition coaches, follow-up calls and using discharge order sets and patient self-care guides (knowledge tools). Successful programs often remain an exception, however, because technical challenges and different organizational cultures make adapting them to other contexts difficult.
Aim: To use the Wiki-suite we have developed to adapt and apply the Acute Care for Elders Program, specifically its care transitions component, in four hospitals in the (CISSS CA) of Quebec.
Focus: Acute geriatric care and care transitions
Jurisdiction: Chaudières-Appalaches region of Quebec
Approach: Our WikiTrauma open-source collaborative database and Wiki 101 training program are designed so that a program can be adapted by the people affected (knowledge users) and then applied (implemented) locally. The "Wiki-suite" was successfully used in adapting trauma care, and now managers and clinicians want to apply it to geriatrics. We will assess the impact of using the Wiki-suite to adapt and apply the ACE Program by asking managers, clinicians and patients about its effects on patient empowerment, health outcomes, and costs. We will also explore how the Wiki-suite works in terms of behavior and organizational change to gain insight into using it to adapt any successful program to any local context (scale up).
Team: Centre intégré de santé et services sociaux de Chaudière-Appalaches, the Institut national d'excellence en santé et services sociaux, the Canadian Foundation for Healthcare Improvement, the Canadian Frailty Network and the Sinai Health System in Toronto.
Peer-reviewed publications and online resources
- Archambault PM et al. 2020. JMIR Research Protocols
- Plaisance A et al. 2018. PLOS One
- Archambault PM et al. 2017. Cochrane Database of Systematic Reviews
- All our publications
- Archambault PM et al. 2018. Canadian Frailty Network. Impact of an online training module and decision aid
- Online training module developed to train intensivists about shared decision making in the ICU
- Decision aid developed to support goals-of-care decision making with older patients in ICU
- Decision aid developed employing user-centred design with the input of patients and ICU clinicians
- Acute Care for Elders (ACE) quality improvement wiki page
-
Dr. Brian Brooks, University of Calgary

Project title: Neurobiopsychosocial outcomes of post-concussion syndrome in youth: Diagnosis, prognosis, and treatment
Embedded Health System Partner: Alberta Children’s Hospital, Alberta Health Service
Brief Bio: Dr. Brian Brooks is a neuropsychologist at the Alberta Children’s Hospital, and an adjunct Assistant Professor in the Departments of Paediatrics and Clinical Neurosciences at the nical Neurosciences at the University of Calgary. His research interests involve the neuropsychological outcome from medical and neurological disorders, including concussion and traumatic brain injury. His research on the neuropsychological outcome from concussions is partially funded by the 2009 McCarthy Tetrault Award. Dr. Brooks was a co-recipient of the 2010 and the 2014 Nelson Butters Awards for the best research papers published in the journal, Archives of Clinical Neuropsychology. He received the National Academy of Neuropsychology Early Career Award in 2014 and also became a fellow of this organization in 2015.
At Issue: Each year, more than 10,000 Canadian children will suffer post-concussion syndrome, which includes long term problems with thinking, headaches, sleep disturbances, depression, social withdrawal, poor quality of life, and lost time at school. When children experience post-concussion, then there is increasing demand on families, schools, and health care organizations. Unfortunately, we understand very little about the causes of post-concussion syndrome and even less about what we can do to treat it.
Aim: My mission is to enhance children's functioning, outcome, and quality of life following concussion (or mild traumatic brain injury).
Focus: The focus of this embedded clinician research program over the next four years is on the children who have post-concussion syndrome; about 10-15% of those who get a concussion.
Jurisdiction: Alberta
Approach: My goals are to: (1) improve our ability to diagnose concussion in youth and determine who will have poor outcome; (2) better understand post-concussion syndrome from biological, psychological, and social viewpoints; (3) determine whether there are long-term effects for youth who sustain concussions; and (4) study new treatment interventions that can reduce symptoms, speed up recovery, or even prevent the post-concussion syndrome. As a clinician within Alberta Health Services and practicing at Alberta Children's Hospital, I am fully embedded with a province-wide health system and am in a unique position to have my clinical research improve quality of care. I am the director of neuropsychology services for this hospital, I meet with hospital management about policy, care, and innovation on a regular basis to dictate strategies for psychology, I am a co-investigator with several members who sit on a provincially based concussion clinical pathways task force, and I have also established several local, national, and international collaborations. Through these avenues I will implement new clinical care pathways and change how care is provide to youth every year.
Research outputs and more information
- Brooks, B et al. 2020, Brain Injury
- Sohn, MN et al. 2020, Journal of the International Neuropsychological Society
- MacMaster F et al. 2020, J Head Trauma Rehabil
- Tomfohr-Madsen L, 2020, J Head Trauma Rehabil
- Brooks, B et al. 2019. Journal of Neurotrauma
-
Dr. Craig Dale, University of Toronto

Project title: Advancing patient-oriented oral care delivery and outcomes in critically ill adults
Embedded Health System Partner: Sunnybrook Health Sciences Centre
Brief Bio: Dr. Craig Dale is an Assistant Professor at the Lawrence S. Bloomberg Faculty of Nursing, Scientist at the University of Toronto Centre for the Study of Pain (UTCSP) and an Advanced Practice Nurse in Adult Intensive Care at Sunnybrook Health Sciences Centre in Toronto.
At Issue: Adverse bacterial and tissue changes in the mouths’ of adults placed on ventilators (breathing machines) can contribute to serious oral discomfort and life-threatening pneumonia. Preventative oral care can lessen these problems but clinicians say this is very difficult to do.
Aim: The overarching goal of my research is to improve the delivery of preventative oral care to a growing population of Canadian adults treated in the intensive care unit (ICU). Approximately 13 million people are admitted to ICUs worldwide each year, and 11% of all Canadian hospitalizations involve time in such units. Growing demand for invasive mechanical ventilation means safe and effective oral care strategies are important.
Focus: Advancing patient-oriented oral care delivery and outcomes is a research program focused on understanding patients’ oral care needs and problem-solving clinicians’ challenges in meeting those needs. This is especially important in the ICU where the nature of critical illness means patients are often unable to give direct input about their care; in turn, clinicians may be unsure about what is appropriate care. As poor oral health is implicated in a range of systemic diseases and poor outcomes, it is important to consider how good oral care can prevent both patient and system level problems.
Jurisdiction: This research will take place in Toronto, Ontario.
Approach: To identify opportunities for improvement, we must integrate the knowledge, experiences, and priorities of ICU patients, families, and health professionals. Our research findings will generate new research questions, interventions to test, and measureable improvements in oral care deemed important to patients.
Team: My team is comprised of patients, family members, nurses, physicians, and dental health professions.
Research outputs and more information
Peer-reviewed articles
- Dale CM, et al. 2020. Trials Journal
- Dale CM et al. 2019. Journal of Clinical Nursing
Knowledge Translation videos
-
Dr. Amit Garg, Western University

Project title: Living Kidney Donation: Embedded Clinician Researcher Program
Embedded Health System Partner: Ontario Renal Network, Trillium Gift of Life Network, Canadian Blood Services, London Health Sciences Centre
Brief Bio: Dr. Garg completed his MD at the University of Toronto in 1995 and received his PhD from McMaster University in 2005 in Clinical Epidemiology & Biostatistics. He is a Professor in the Departments of Medicine (Nephrology), Epidemiology & Biostatistics at Western University, and is a nephrologist and Director of Living Kidney Donation at the London Health Sciences Centre. He also holds an appointment in the Department of Clinical Epidemiology and Biostatistics at McMaster University. He is the lead on the Provincial Institute for Clinical and Evaluative Studies (ICES) Kidney, Dialysis and Transplantation Program and Director of ICES@Western. He is the current President of the Canadian Society of Nephrology, and is the Ontario Medical Lead for Access to Kidney Transplantation and Living Donation for the Ontario Renal Network / Trillium Gift of Life Network.
At Issue: Patients with kidney failure often wait years to receive a new kidney. Many patients die while they are waiting. There is a small amount of risk for a living person who is healthy to donate one of their kidneys – called Living Kidney Donation. Unfortunately, many patients who would benefit from a kidney transplant do not receive one. There are many reasons for this. Doctors do not always talk to their patients about transplantation. Patients are often uncomfortable discussing living kidney donation with family and friends. Many people do not realize they will remain in good health if they donate a kidney; some are told they are too old to donate despite new research showing it is safe if they are healthy. As well, donor evaluation often takes a year to complete (when it should only take 3 months). Canada and other countries are looking for ways to safely increase living kidney donation.
Aim: To enable more patients with kidney failure to safely receive transplants, and help candidates make informed decisions about becoming living kidney donors.
Focus: Addressing barriers to Living Kidney Donation
Jurisdiction: The program of research activities are provincial, national and international.
Approach: My research team is working with living kidney donors and transplant programs to develop and test solutions to overcome barriers to living kidney donation. As well, we are studying a large group of living kidney donors over many decades to confirm long-term safety.
Team: Patients, healthcare providers, research methodologists, trainees, healthcare organizations (Ontario Renal Network Trillium Gift of Life Network, Canadian Blood Services)
More information: Please contact amit.garg@lhsc.on.ca
-
Dr. Sara Guilcher, University of Toronto

Project title: Characterizing care transitions for complex populations using patient-centred episodes of care and evaluating solution-focused targeted interventions
Embedded Health System Partner: Health Quality Ontario
Brief Bio: Sara is an Assistant Professor at the Leslie Dan Faculty of Pharmacy, an Adjunct Scientist at the Institute for Clinical Evaluative Sciences, Affiliate Scientist at the Centre for Urban Health Solutions, St. Michael’s Hospital, and an Investigator with the Health System Performance Research Network (HSPRN). She completed her BSc (Hons) in Bio-psychology at Mount Allison University in 2001 and her MSc in Physical Therapy at the University of Toronto in 2003. She completed her MSc in Psychology (Clinical) at Western University in 2006 and her PhD in Clinical Epidemiology in the Institute of Health Policy, Management and Evaluation at the University of Toronto in 2012. Dr. Guilcher completed a two year post-doctoral CIHR funded fellowship in the Action For Health Equity Interventions (ACHIEVE) program at St. Michael’s Hospital, and a former trainee with HSPRN. Sara’s overall research is to improve health service delivery across the continuum of care, specifically for marginalized populations with complex health and social needs.
At Issue: Transitions from one sector of the health care system to another are the most dangerous and vulnerable periods for patients and caregivers. Therefore, improving transitions and related experiences are major foci of quality improvement initiatives in most health jurisdictions within Ontario, Canada and globally. Transitions involve care across different providers, and it is essential to use a patient perspective and measure individuals' transitions over time. Further, in order to improve transitions of care, it is necessary to understand the contextual factors surrounding transitions throughout transitions of care.
Aim: To: (1) characterize trajectories for complex populations through patient-centred episodes of care using administrative health data; (2) understand patient, caregiver, provider and decision-maker experiences for health system performance improvement using qualitative methods; and (3) identify and evaluate quality improvement interventions to optimize transitions in care for complex populations.
Jurisdiction: This work is primarily set in Ontario but has relevance to other jurisdictions.
Approach: Given rising health care costs, it is increasingly important to provide efficient value-based health care that is needs driven for specific populations across the continuum of care. Working with Health Quality Ontario, this innovative research will inform opportunities for system improvement for targeted interventions, such as the creation of potential payment bundling options for care episodes among different complex populations. In understanding trajectories for persons with complex needs, transformational models of care can be co-created with patients and providers to encompass the entire anticipated expected trajectory of care for optimal service delivery and outcomes.
Research outputs and more information
- Lake JD, et al. 2020. BMC Health Services Research
- Guilcher SJT, et al. 2020. BMC Health Services Research
- Tessier L, et al. 2019. CMAJ
- Asif M, et al. 2019. Journal of Disability and Rehabilitation
- Everall A, et al. 2019. Health Expectations
-
Dr. Catherine Hudon, University of Sherbrooke

Project title: Frequent users of health services with chronic conditions likely to require ambulatory care: Better identifying clients at risk to better intervene
Embedded Health System Partner: Ministère de la Santé et des Services sociaux du Québec [Quebec department of health and social services] and Centres intégrés universitaires de santé et de services sociaux du Saguenay–Lac-St-Jean et de l’Estrie [integrated university health and social services centres of Saguenay–Lac St-Jean and Estrie].
Brief Bio: Dr. Hudon completed her medical training at Laval University in 1996, and then completed a certification in family medicine at the University of Sherbrooke in 1998. She has been a member of the College of Family Physicians of Canada since 1998. She completed a master’s degree in clinical sciences in 2004, a transdisciplinary fellowship in primary health care research in 2006 and a doctoral degree in clinical sciences at the University of Sherbrooke in 2012. She is a full professor with the department of family medicine at the University of Sherbrooke. Dr. Hudon’s research interests are focused on the integration of services and self-management support for patients with complex needs who are at risk of being frequent users of health services.
At Issue: Some people with chronic diseases also have psychological and/or social problems that increase their needs with regard to the health system. For a small portion of these individuals, the services provided do not adequately meet their needs, and they very often consult emergency services and other health services without necessarily receiving the services they would have needed. Case management is an intervention that could help them while improving the integration of services. However, it is important to properly identify the clients who could benefit the most from a case management intervention.
Aim: This research program, which was developed in partnership with the Direction de l'organisation des services de première ligne intégrés [integrated primary care services organization branch] of the Ministère de la santé et des services sociaux du Québec, with the Centres intégrés universitaires de santé et de services sociaux du Saguenay–Lac-St-Jean et de l’Estrie, aims to better identify patients with chronic diseases who are at risk of being frequent users of health services to offer them a case management intervention that could better meet their needs.
Jurisdiction: This research program, which is currently being deployed at the provincial level, is in the process of developing national collaborations.
Approach: In addition to producing new scientific knowledge that could be useful in other contexts in Quebec, Canada and abroad, this research program will have several direct impacts on the health care system. Changes will be made to existing case management programs to improve the care experience of patients and the integration of resources. Decision makers and the Ministère will be better informed to plan the organization of services for this clientele, and a clinical tool will be integrated into the computerized clinical file to more quickly identify patients who should receive care better adapted to their needs.
Team: Various key stakeholders are involved in our work: patient partners, decision makers, managers, clinicians and researchers. This program is part of the Quebec SPOR SUPPORT Unit’s demonstration project.
Research outputs and more information
Peer-reviewed publications
- Hudon C et al. 2017. BMJ Open
- Danish A et al. BMJ Open
- Dufor I. et al. 2020. Geriatrics Gerontology
- Depelteau A et al. 2020. American Journal of Emergency Medicine
- Vanasse A et al. 2020. BMC Health Services Research
For any additional contact or information: Catherine.Hudon@Usherbrooke.ca
-
Dr. Naana Afua Jumah, Northern Ontario School of Medicine

Project title: Addressing Transitions in Care: An Indigenous-based, Integrated Care Pathway for Opioid Dependence in Pregnancy in Northwestern Ontario
Embedded Health System Partner: Thunder Bay Regional Health Sciences Centre
Brief Bio: Dr. Jumah has an undergraduate degree in Chemical Engineering from the University of Toronto, a PhD in Medical Engineering from Oxford University and an M.D. from Harvard Medical School. She completed a five-year residency in Obstetrics and Gynecology in Toronto and a one-year fellowship specializing in the management of addictions during pregnancy, working with Dr. Meldon Kahan, an addiction specialist at the University of Toronto’s Department of Family and Community Medicine. In 2014, Dr. Jumah returned to her hometown to take on a dual role as both a clinician and researcher at the Thunder Bay Regional Health Sciences Centre and its affiliated research institute.
At Issue: Opioid use affects up to thirty percent of pregnancies in Northwestern Ontario. Accessing appropriate care during pregnancy and after birth can be overwhelming especially for women with substance use issues living in rural and remote communities who are forced to travel from their home community to a maternity centre for confinement, delivery and post-partum while the infant receives care for the neonatal abstinence syndrome. The availability of health and social services vary widely in Northwestern Ontario and health care providers have varying comfort levels providing care to substance using pregnant women. Furthermore, practitioners and programs in Northwestern Ontario often work in isolation with little inter-sectoral and inter-organizational communication. As a result, there is often little to no continuity of care as the patient moves between communities. First Nations women have the additional layer of complexity in that they also have to navigate both federal and provincial healthcare systems.
Aims:
- To develop evidenced-based standards of care for the management of pregnant women with substance use issues who live in rural and remote areas
- To implement and assess health system change based on community derived interventions for opioid dependent pregnant and parenting Aboriginal women and their children
- To explore the role and interplay of tele-obstetrics, tele-mental health and tele-addictions along with web-based tools in the management of substance using pregnant and parenting women
Focus: Substance using pregnant women living in rural and remote areas
Jurisdiction: Northwestern Ontario
Approach: Community driven participatory research
Team Members: Maternal Addictions Continuum of Care (MACC) Project (Shibogama First Nations Health Authority), Lisa Bishop (Aboriginal Midwife)
-
Dr. Gilaad Kaplan, University of Calgary

Project title: Innovating Healthcare Delivery to Manage the Rising Prevalence of the Inflammatory Bowel Diseases
Embedded Health System Partner: Alberta Health Service’s Digestive Health Strategic Clinical Network – an evidence-based province-wide initiative that will reduce variations in clinical practice and ensure equitable access to high quality care for every Albertan with IBD.
Brief Bio: Dr. Kaplan is a gastroenterologist and epidemiologist with a clinical and research interest in the inflammatory bowel diseases (IBD). He graduated with a Masters of Public Health from the Harvard School of Public Health and completed an IBD Fellowship at the Massachusetts General Hospital. He is an Associate Professor in the Cumming School of Medicine at the University of Calgary. He is an Alberta-Innovates Health Solutions Population Health Investigator and the Scientific Director of Alberta Health Services’ Digestive Health Strategic Clinical Network. Dr. Kaplan was selected as one of Avenue Calgary Magazine's Top 40 Under 40 (2011), the Canadian Association of Gastroenterology’s Young Investigator (2013), and the University of Calgary’s Killam Emerging Research Leader (2013).
At Issue: Approximately 0.5% of Canadians are diagnosed with the inflammatory bowel diseases (IBD), which consists of Crohn's disease and ulcerative colitis. In Canada, we lose $3 billion a year from the cost of IBD. Because ulcerative colitis and Crohn's disease are chronic, incurable diseases of the young, the number of people afflicted by IBD continues to steadily rise in Canada.
Aim: To prepare Alberta's healthcare system to meet the challenges that patients with IBD and society will face over the next decade from the rising burden of IBD.
Jurisdiction: The province of Alberta, and Alberta Health Services
Approach: We will build models that predict the future needs to care for patients with IBD and then implement innovations in healthcare delivery that will improve the quality of care for patients with IBD. Strategies for care redesign will involve building an integrative model of care between primary care physicians and gastroenterologists, designing an electronic referral system that will standardize triage for patients with IBD and identify individuals for rapid diagnosis of IBD, enhancing access to care for underserviced areas, and improving transition from hospital to home for patients with IBD.
Team Members: Blair O’Neil, Associate Chief Medical Officer, Strategic Clinical Network, Alberta Health Services; Linda Slocombe, Medical Director, Calgary Foothills Primary Care Network; Jodi Glassford, Director, Provincial Access Team, Alberta Health Services; Aida Fernandes, Vice President, Crohn’s and Colitis Canada
Research outputs and more information
Access the talk titled “Investigating the causes of a modern disease of modern times”
Dr. Kaplan wrote an essay that predicted the evolution of the globalization of IBD from 2015-2025. Nature Reviews: Gastroenterology & Hepatology [2015;12(12):720]
Dr. Kaplan led a study that revealed the rising incidence of IBD in the Western world and its emergence in newly industrialized countries [Gastroenterol. 2012;142(1):46]. This is the most cited paper in Gastroenterology over the past 5 years with over 1500 citations (source: Google Scholar).
Other peer-reviewed publications
- Coward S et al. 2019. Gastroenterology
- EI Benchimol, et al. 2019. Journal of the Canadian Association of Gastroenterology
- Kaplan GG*, et al. 2019. CMAJ
- JA King, FE et al. 2019. The Lancet Gastroenterology & Hepatology
- SC Ng, et al. 2017. The Lancet
-
Dr. Tara Kiran, St. Michael’s Hospital

Project title: Measuring quality of care for patients discharged from hospital to home
Embedded Health System Partner: Health Quality Ontario (HQO)
Brief Bio: Dr. Kiran is a Staff Physician and Assistant Professor in the Department of Family and Community Medicine, St. Michael’s Hospital, University of Toronto. She is an Associate Scientist in the Centre for Urban Health Solutions, Li Ka Shing Knowledge Institute, St. Michael’s Hospital and an Adjunct Scientist at the Institute for Clinical Evaluative Sciences. Dr. Kiran has held numerous advisory roles with local and provincial government. She was the Provincial Clinical Lead for the Ontario Diabetes Strategy with the Ministry of Health and Long-Term Care and has also served as a Primary Care Advisor for the Toronto Central Local Health Integration Network. She is currently the Board Chair for the St. Michael’s Hospital Academic Family Health Team. Dr. Kiran’s research evaluates the impact of primary care reforms in Ontario.
At Issue: Research has demonstrated that the care people receive when transitioning out of hospital is often fragmented and puts them at risk of developing complications. Yet, we currently do not have good ways of measuring and reporting on this care. Measuring the quality of care is a necessary step for improvement.
Aim: First, to develop a set of quality measures that assess how good the care is for people admitted to hospital and discharged home. Second, to test whether using these measures for public reporting or quality improvement results in better care.
Jurisdiction: The research will be conducted in Ontario.
Approach: Our research program will begin by asking members of the public what they think are the most important aspects of care for people transitioning from hospital to home. We will also look at what existing research says can be done to improve this care. We will use the feedback and research findings to develop a "Quality Standard" that outlines what good care looks like when people are discharged home from hospital. The Quality Standard will include 5 to 15 concise, specific recommendations. Each recommendation will be accompanied by a set of measures that can help organizations assess whether they are providing excellent care. Once we develop the measures, we will assess whether it is feasible for Health Quality Ontario (HQO) to collect and report some of them systematically for hospitals, primary care practices, and home care organizations in Ontario. We will consider which of these measures should be reported directly to the public, which should be reported to organizations privately, and which would be most useful to spur local improvements in care. We will then conduct a large research study to evaluate the impact of having HQO i) publicly report measures and ii) prioritize measures for local quality improvement. We will assess whether these changes result in improvements to the quality of care for people discharged from hospital to home.
Research outputs and more information
- Op-ed article on homecare during the COVID-19 pandemic in The Star, “We need to strengthen publicly funded homecare in time for winter”, July 20, 2020.
- Kiran T et al. 2020. CMAJ Open.
- Kiran T et al. 2020. BMJ Quality and Safety.
- Dainty K, Kiran T. 2020. British Journal of General Practice Open
- Hsu J, et al. 2019. Psychiatric Services
- Lofters A, et al. 2019. Journal of General Internal Medicine
- Lavergne R, et al. 2019. BMJ Open 2019
-
Dr. Martha Mackay, University of British Columbia

Project title: Transitions in care: Improving outcomes for cardiac patients
Embedded Health System Partner: St. Paul’s Hospital, Providence Health Care
Brief Bio: Dr. Martha Mackay is currently a clinician-scientist, dividing her time between the roles of Clinical Nurse Specialist (CNS) in Cardiology at St. Paul’s Hospital’s Heart Centre and Clinical Associate Professor at the University of British Columbia (UBC) School of Nursing. She has been practicing for more than 38 years in critical care and cardiac nursing, with many years as a critical care nursing educator, and 20 years as a CNS. Her initial nursing education was at George Brown College in Toronto, and she has since earned her BSN, MSN and PhD (2010) degrees at UBC.
At Issue: Transitions in care occur when patients move from a hospital to home or another site of care. Another critical transition in heart care is when heart attack patients seek care at a hospital. Such transitions are known to be a time of increased risk for all patients, and cardiac patients are no exception. These risks may be related to insufficient information being provided to the patient and family, inadequate planning for follow-up care, or patients' or caregivers' lack of required knowledge and skill to manage the transition. Poor transitions can lead to more emergency department visits and hospital admissions, as well as unnecessary suffering.
Aim: To address some of the critical transition points in cardiac care
Focus: Patients with unique and underappreciated needs. In particular, the research program will focus on overcoming ethnicity-based barriers to seeking and receiving care for heart attacks, improving access to depression care for affected heart patients, and enhancing understanding of, and adherence to, discharge instructions.
Jurisdiction: British Columbia. My research will enrol patients from across the province who come for care at St. Paul’s Hospital Heart Centre.
Approach: A variety of approaches will be used. Some work will involve observation of care as it is occurring, and interviews with patients to identify gaps or discrepancies. Some work will involve clinical trials of novel ways of treating heart patients. For example, treatment for cardiac patients who also suffer from depression, or reminders about discharge instructions after a heart attack, sent for weeks or months after discharge. Both of these interventions which will use telehealth methods to improve access for patients.
Team: We are working with a patient advisor on both our depression and discharge messaging studies, and will be engaging with family physicians in the near future about improving communication between them and the acute care hospital after their patients have been hospitalized.
Some Members of My Research Teams Include:
Dr. Quincy Young (Clinical Psychologist, St. Paul’s Heart Centre; Dr. Scott Lear, Heart & Stroke/Pfizer/St. Paul’s Hospital Foundation Chair in Preventive Cardiology Research, Simon Fraser University; Dr. Joel Singer, Professor, School of Population and Public Health, UBC; Dr. Susan Abbey, Professor (Psychiatry), University of Toronto and Psychiatrist-in-Chief, University Health Network; Dr. Pamela Ratner, Vice-Provost and Associate Vice-President, Enrollment and Academic Facilities, UBC; Dr. Karin Humphries, Associate Professor, Faculty of Medicine (Cardiology), UBC; Director, Centre for Improved Cardiovascular Health, Vancouver, BC; Dr. Gerry Veenstra, Professor, Faculty of Sociology, UBC; Dr. Frank Scheuermeyer, Clinical Assistant Professor (Emergency Medicine), UBC & Staff Physician, Providence Health Care; Dr. Krishnan Ramanathan, Clinical Assistant Professor (Cardiology), UBC & Director, Cardiac Intensive Care Unit, St. Paul’s Hospital; Dr. Min Gao, Clinical Assistant Professor, UBC; Dr. Nichole Pugh, Registered Clinical Psychologist, Research Associate, Yale University
Research outputs and more information
- Doson C et al. 2019. Canadian Journal of Cardiology
- Mackay MH et al. 2018. Academic Emergency Medicine
- Iacoe E et al. 2017. European Journal of Cardiovascular Nursing
- Ross ES et al. 2017. JMIR Res Protoc.
-
Dr. Geoffrey Nguyen, University of Toronto

Project title: A national network to improve access and quality of care for those with inflammatory bowel disease
Embedded Health System Partner: Mount Sinai Hospital (part of Sinai Health System)
Brief Bio: Dr. Nguyen is an Associate Professor of Medicine at the University of Toronto and the Institute for Health Policy Management and Evaluation. He is also adjunct faculty at the Johns Hopkins School of Medicine and an adjunct scientist at the Institute for Clinical Evaluative Sciences in Toronto. After graduating from the Johns Hopkins School of Medicine in 2000, he completed residency in Internal Medicine at the Johns Hopkins Hospital in 2003. He then pursued a combined clinical and research fellowship in gastroenterology at Johns Hopkins. He concurrently completed a PhD degree in Clinical Investigation at the Johns Hopkins Bloomberg School of Public Health in 2007 under the auspices of an NIH-sponsored National Research Services Award. The main focus of his research is the impact of IBD specialty care on health outcomes at the population level.
At Issue: Inflammatory bowel disease (IBD) is a chronic condition that is more common in Canada than most other parts of the world. Patients with inflammatory bowel disease benefit from the care of a gastroenterologist early in the course of disease who may help to optimize care and thus reduce the need for surgery. Among the gaps in the care of IBD patients is lack of access to specialist care and suboptimal quality of care. The overuse of chronic systemic steroids is especially problematic.
Aim: The Promotion of Access and Care through Centres of Excellence (PACE) Program’s main goal is to improve quality of IBD care in underserved communities by increasing their access to specialists.
Focus: The PACE program focuses on inflammatory bowel disease but the model for improvement can hopefully be applied to other chronic diseases.
Jurisdiction: The PACE Program will have national reach and will implemented at 5 of the largest IBD Centres of Excellence in Canada (Mount Sinai Hospital at the University of Toronto; McMaster University, McGill University, University of Alberta, University of Calgary).
Approach: The program’s goals will be achieved through the use of telemedicine, standardized clinical care pathways, and web-based remote monitoring of patients. PACE will measure the success of its interrelated initiatives through the development and measurement of quality indicators tailored to the program.
Team: Aside from physician stakeholders from the 5 IBD Centres of Excellence, PACE is sponsored by Crohn’s and Colitis Canada (CCC) which is national advocacy group for inflammatory bowel disease and represents patient stakeholders. The program is also partnered with the Ontario Telemedicine Network that provides the infrastructure for telemedicine-based clinical visits. PACE is also a member of the HealthPROMISE consortium which enables the technology to remotely monitor patient disease status.
Research outputs and more information
- Habashi P, et al. 2018. J Can Assoc Gastroenterol
- Bitton A, et al. 2019. Inflamm Bowel Dis
- Nguyen GC, et al. 2019. J Crohns Colitis
-
Dr. Tracey Rickards, University of New Brunswick

Project title: Sealing the cracks for priority populations with the Fredericton Downtown Community Health Centre
Embedded Health System Partner: Fredericton Downtown Community Health Centre
Brief Bio: Dr. Tracey Rickards is an RN with clinical and research expertise and a keen interest in vulnerable populations. She is an Assistant Professor in the Faculty of Nursing at the University of New Brunswick in Fredericton. Dr. Rickards completed her Bachelor of Nursing at UNB in 1986, her Master's of Nursing at UNB in 2005, and her PhD in Nursing at Dalhousie University in 2013. She has worked as a nurse for 30 years holding a variety of positions, and has been involved with the Fredericton Downtown Community Health Centre for over a decade.
At Issue: Vulnerable populations include people who are, or at risk of, becoming homeless, marginalized because of their social status, immigrant status, age, or other defining features, and living with more than one illness requiring significant health care. They often "fall through the cracks" in preventive and on-going health care management resorting to emergency room care when they get sick.
Aim: As the Embedded Clinical Researcher (ECR) Dr. Tracey Rickards will connect research, clinical reality, and community to show how collaboration in an urban community health centre can improve health outcomes for vulnerable populations and try to decrease health care costs.
Focus: The focus of research is: adequate housing to achieve stable health for vulnerable populations, nurses impact on health outcomes to decrease health care costs, outreach care for the most vulnerable clients, and evaluation of the Nurse Practitioner role in New Brunswick. These priority goals will drive the ECR while building a strong culture of research at the Fredericton Downtown Community Health Centre (FDCHC).
Jurisdiction: Fredericton, New Brunswick
Approach: As the ECR, Dr. Rickards will mentor novice nurses and researchers/teams, as well as examine how full scope of practice for both nurses and Nurse Practitioners can impact the health practices of vulnerable populations and decrease visits to emergency rooms and how interdisciplinary collaboration can support positive preventive health care experiences. The results will give clear direction for effective use of resources for governments and institutions as health care costs continue to increase. In this four-year CIHR funded project, Dr. Rickards will develop clinically relevant research and a strong research team within the FDCHC who will do transformative and innovative research.
Team: Dr. Tracey Rickards will work with a multi-disciplinary team at the Fredericton Downtown Community Health Centre to identify research questions. The FDCHC has a strong partnership with Horizon Health Network. The team will also include the input of clients who use the FDCHC. Further to this there are a number of organizations serving the Fredericton population who will be included as partners in various research projects. Some of these organizations include but are not limited to: The Fredericton Emergency Shelter, The Community Kitchen, mental health services, AIDSNB, Multicultural Association of New Brunswick, the John Howard Society, Fredericton Police, etc.
Research outputs and more information
- Rickards, T et al. 2018. SAGE Open Access
- Rickards, T and Hamilton S. 2019. Journal of Nurse Practitioners
- Hamilton, S, and Rickards, T. (2018). Info Nursing
- Rickards, T. & Kitts, E. (2018). Canadian Journal of Respiratory Therapy
-
Dr. Robert Schroth, University of Manitoba

Project title: Improving access to oral health care and oral health care delivery for vulnerable young children in Manitoba
Embedded Health System Partner: Winnipeg Regional Health Authority*, Manitoba Health, Seniors and Active Living, Mount Carmel Clinic, Manitoba Dental Association, and Children’s Hospital Research Institute of Manitoba
*contributing required funding
Brief Bio: Dr. Schroth is presently an Associate Professor and Clinician Scientist in the Department of Preventive Dental Science (College of Dentistry) and the Departments of Pediatrics & Child Health and Community Health Sciences (Max Rady College of Medicine), Rady Faculty of Health Sciences at the University of Manitoba. He is also a research scientist at the Children’s Hospital Research Institute of Manitoba. In July 2016 he was appointed Section Head of Pediatric Dentistry for the Winnipeg Regional Health Authority. He holds a PhD with training in Epidemiology, Population Health, and Community Health Sciences and has an established research program on Early Childhood Caries (ECC), oral health promotion and program evaluation, and health services research relating to pediatric dental surgery to treat severe ECC. Naturally, there is a strong focus on Indigenous (First Nations and Metis) children’s oral health. Some of his work has examined the role of prenatal factors, including vitamin D levels, on the oral health of infants and preschool children. He also co-leads a large early childhood oral health promotion project in Manitoba, Healthy Smile Happy Child, which includes a considerable research and evaluation component He is recognized as a leading national expert on the subject of ECC. In 2009-2010 he was appointed to the Canadian Dental Association’s (CDA’s) Working Group and Task Force on ECC and co-authored the CDA’s new position statement on ECC. More recently, he was appointed to the Canadian Institute for Health Information (CIHI) Expert Panel for the analysis on day surgery for ECC and co-authored their report and led a journal publication on this work. From 2003-2007 he was a CIHR Strategic Training Fellow in the Child Health Clinician Scientist Program (CCHCSP).
At Issue: Significant oral health disparities exist in Canada. Nowhere is this more evident than among children from vulnerable populations including low-income households, First Nations, Metis, and Inuit peoples, refugees and recent immigrants, and children living in rural and remote regions of the country. Unfortunately, poor access to oral health care for our youngest members of society often manifests itself as early childhood caries (ECC). Further, we know that those who then develop severe forms of ECC and require comprehensive dental surgery face additional barriers to accessing timely dental care under general anesthesia. Increasing access to early oral health care for vulnerable groups of children is critical in order to curb the incidence of ECC.
Aim: Since good oral health during early childhood sets the foundation for a lifetime of optimal dental and total health, my proposed program of research aims to improve access to oral health care for young children at-risk for ECC and improve oral health care delivery for children requiring dental surgery to treat their ECC.
Focus: The first project looks at rates of dental surgery as a proxy for poor oral health arising from a failure of access to early preventive dental care for young infants, toddlers and preschool children. The second proposed project will address concerns relating to wait times, wait lists, and the need to improve oral health service delivery in Manitoba for children with S-ECC requiring rehabilitative dental surgery.
Jurisdiction: Manitoba
Approach: My vision as an embedded clinician research includes 4 elements: 1) Research that strives to improve the oral health status and oral health quality of life of our youngest members in society by focusing on ways to improve access to oral health care and oral health care delivery; 2) Mentorship that builds capacity for future oral health and health services research and clinical leadership; 3) Integrated knowledge translation and exchange; and 4) Collaborations and partnerships with health system organizations and decision-makers to bridge the gap between research, practice, and policy.
Team: I am partnering with the Winnipeg Regional Health Authority, Manitoba Health, Seniors and Active Living, Mount Carmel Clinic, the Manitoba Dental Association, and the Children’s Hospital Research Institute of Manitoba.
Research outputs and more information
- Almoudi MH, et al. 2019. Pediatr Int
- Bonnet C, et al. 2019. J Can Dent Assoc
- Day G, et al. 2019. J Dent Res
- Wong JP, et al. 2019. J Fam Pract
- Grant CG, et al. 2019. Pediatr Dent
-
Dr. Marie-Josée Sirois, Université Laval

Project title: Assessing the effectiveness of the “CEDeComS intervention” on reducing functional decline in seniors presenting with minor injuries
Embedded Health System Partner: Centre intégré universitaire de santé et de services sociaux (CIUSSS) de la Capitale Nationale
Brief Bio: Pr. Sirois is an Associate Professor in the Department of Rehabilitation in the Faculty of Medicine at Laval University and researcher at the Centre d’Excellence sur le Vieillissement de Québec. She has co-lead the CIHR-funded Canadian Emergency and Trauma Initiative in elders (CETIe), a multicenter interdisciplinary team studying the consequences of trauma in seniors through large prospective cohorts. Based on a combined focus on identifying the multidimensional determinants of post-injury function in seniors, and on implementing new knowledge in clinical practice, the CETIe aims to improve the acute care and management of this population. Pr Sirois specializes in the assessment and management of frailty in seniors with injuries. She currently works on innovative solutions to improve care transitions between Emergency Departments and community settings in order to prevent functional losses in pre-frail/frail injured seniors. She is a member of the Réseau Québécois de Recherche sur le Vieillissement (RQRV).
At Issue: Each year in Canada, nearly 500 000 community-dwelling seniors sustain injuries that are not fatal but that limit their mobility and daily activities. The vast majority of these seniors seek medical care in Emergency Departments (EDs) and two-thirds are discharged back home with various minor injuries. Evidence generated by the Canadian Emergency Team Initiative (CETI), has shown that these minor injuries can trigger a downward spiral of functional decline (in mobility and daily activities) in 16% of seniors who are still independent at the time of their injury. Moreover, these injuries unmask early signs of impairments as well as a pre-frail/frail status. As there are no ED management guidelines designed to prevent these injured seniors from losing their mobility and function, they deteriorate within 6 months post-ED discharge. This is unfortunate as there is compelling evidence of the effectiveness of community-based mobility interventions in improving frailty & function. Such interventions include fall prevention & exercise programs, which are available across all Canadian communities. In that context, identification of seniors at risk of functional decline is crucial in EDs to implement effective interventions.
Aim: The main objective of this study is to assess the effectiveness of the “CEDeComS intervention” on reducing functional decline in seniors presenting to the ED with minor injuries.
Approach: The CETI has validated a Clinical Decision Rule (CETI-CDR) to screen & orient seniors at high, moderate & low risk of decline to appropriate post-ED follow-ups. We thus propose the new CEDeComS intervention that combines CETI-CDR screening with rapid linkage to mobility programs in the community, directly from the ED. The study builds on the formation of new ED-community partnerships that will improve the care continuum to help these seniors remaining independent.
Research outputs and more information
- Martel D, et al. 2018. Experimental Gerontology
- Blouin M, et al. 2018. J Gerontol & Geriatric Research
-
Dr. Erna Snelgrove-Clarke, Dalhousie University

Project title: Maternal Obesity in Atlantic Canada: Implementing evidence into clinical practice
Embedded Health System Partner: IWK Health Centre
Brief Bio: Dr. Snelgrove-Clarke is an Associate Professor in the School of Nursing and the Department of Obstetrics & Gynecology at Dalhousie University. She is a registered nurse and completed her Bachelor of Nursing at Memorial University of Newfoundland, her Master of Nursing at Dalhousie University and PhD at McGill University. Her area of clinical practice focuses on perinatal nursing and her program of research focuses on the identification of successful strategies for the use of evidence in clinical practice; concentrating on understanding the context and changing behavior amongst health care providers in Maternal and Newborn Health thereby improving patient outcomes.
At Issue: Obesity is a serious global health problem. Nearly 60.6% of Canadian adults are overweight or obese, with rates having doubled in some parts of Canada in just two decades. Atlantic Canada has among the highest rates of obesity in Canada. More specifically, as demonstrated in the Canadian Maternity Experiences Survey, women in Nova Scotia have the highest average prepregnancy body mass index. Associated with obesity are a number of important safety and financial implications for health care professionals and the health system.
Aim: In an effort to improve the health of these childbearing women in Nova Scotia, our goal in this research project is to implement and evaluate two clinical practice initiatives, a clinical practice guideline and a best practice model. These initiatives provide evidence-based recommendations for the care of women that are obese prior to and during their labour and birth. In addition, we also are focusing on gestational weight gain during pregnancy and its impact on pregnancy and labour, and birth outcomes.
Focus: Our health care system is struggling to manage and provide proper care for the rising numbers of pregnant patients living with obesity who are frequently affected by a number of comorbidities. There are serious health and safety risks to health care workers associated with lifting and moving obese patients, including back and soft tissue injuries.
Jurisdiction: Nova Scotia
Approach: Strategies to influence change on the behaviour of health care professionals and to enhance the health of consumers are influenced by a variety of factors. In addition, we will need to understand more about the setting since successful behavior is influenced by the context where care is provided. In this case, the areas where both prenatal and labour and delivery care are provided to women. We will also need to work with all health care providers employed in these settings to make sure that the strategies we use to bring about change are the best for everyone. Through this study, we will begin to not only improve the surveillance of management of this population, but also identify ways to improve education, practice, policy, and research in the area of management for obese women giving birth in Nova Scotia. The impact of this project will lead to approaches for influencing behavior change in other care areas for pregnant women.
Team: This team will be comprised of clinicians (obstetricians, obstetrical residents, nurses, midwives, dietician), decision makers (clinical managers, program director), students (undergraduate and graduate health professional students), and consumers.
Co-Applicants/Team Members: In order to be inclusive and collaborative, I will announcing the team once all co-applicants have been approached.
More information:
-
Dr. Carolyn Snider, University of Manitoba

Project title: Development, Implementation and Evaluation of Interventions for Youth Injured by Violence
Embedded Health System Partner: Winnipeg Regional Health Authority
Brief Bio: Dr. Snider is an emergency physician in the Winnipeg Regional Health Authority, Associate Professor in the Department of Emergency Medicine, College of Medicine at the University of Manitoba and a Scientist at the Children's Hospital Research Institute of Manitoba. She has a strong track record in applying multiple methodologies to approach the chronic health problem of youth violence.
At Issue: Approximately 20% of youth who are injured by violence will visit an emergency department in the next year with a recurrent intentional injury. Youth at risk of violence are also at high risk of addictions and mental health conditions.
Aim: To reduce repeat injury, along with substance use and mental illness among youth injured by violence will have a substantial financial and social benefit to our health care system.
Focus: To develop, implement and evaluate an emergency department-initiated violence intervention for youth injured by violence.
Jurisdiction: The current ED-based violence intervention (EDVIP) is based in Winnipeg, Manitoba with a goal to help other jurisdictions implement their own EDVIP and involve them in future evaluation. Dr. Snider collaborates with similar programs in the United States on research. Additionally, Dr. Snider is currently completing a manual for the World Health Organization on the role of emergency medicine in violence prevention.
Approach: In 2013, Dr. Snider launched the Emergency Department Violence Intervention program (EDVIP) study. EDVIP is a unique care program that uses a wraparound care model delivered by a support worker with lived experience with violence, assisted by a social worker and links to multiple community services. Dr. Snider uses integrated knowledge translation throughout her research to ensure that interventions are relevant to the community. She employs observational, randomized control trial as well as qualitative methodologies to understand the key risk and protective factors of youth violence and to design, implement and rigorously evaluate interventions. Dr. Snider has developed an international reputation for her research and is translating her research to policy at the World Health Organization.
Team: The team includes includes clinicians, researchers, community youth workers and Aboriginal Elders. Three Aboriginal youth who had been former gang members had an active role in developing and adapting the EDVIP intervention. Current EDVIP support workers are all Indigenous from various communities. We follow the First Nations OCAP principles of doing research with Aboriginal people and have partnership on the EDVIP project with the Assembly of Manitoba Chiefs.
Team Members: University of Manitoba: Drs. Terry Klassen, Depeng Jiang, Wanda Chernomas, Elaine Mordoch, Evelyn Forget, Rick Linden, Mr. Trevor Strome and Ms. Karen Cook. Winnipeg Regional Health Authority: Drs. Natalie Mota, Katie Sullivan, Sarvesh Logsetty. Government of Manitoba: Dr. Rob Santos, Leanne Boyd. Gang Action Interagency Network: Jamil Mahmood. Assembly of Manitoba Chiefs: Carla Cochrane. Advisory Committee: includes over 25 community and clinical colleagues which meets 3 times per year.
Research outputs and more information
- Successes are highlighted in this video
- Snider et al. 2020. Canadian Journal of Emergency Medicine
-
Dr. H. Tom Stelfox, University of Calgary

Project title: Journey out of intensive care: re-engineering return to the community
Embedded Health System Partner: Alberta Health Services
Brief Bio: Dr. H. Tom Stelfox is an Associate Professor of Critical Care Medicine, Medicine and Community Health Sciences at the University of Calgary. He received his M.D. from the University of Alberta, Internal Medicine Residency at the University of Toronto, Ph.D. in Health Care Policy at Harvard University and Critical Care Fellowship at the Massachusetts General Hospital. His research program focuses on the application of health services research methods to evaluate and improve the quality of health care delivery to critically ill patients. His research activities include developing quality indicators in trauma care; evaluating the structure and transfer of knowledge in hospitalized patients; and evaluating new health care technologies, risk stratification tools and methods of health service delivery.
At Issue: When patients are transferred from one care setting to another there is a high risk of error. The discharge of patients from the intensive care unit (ICU) is an example of a high-risk transfer. These are the sickest and most complex patients. For the past four years I have led a team of professionals and interested citizens to re-design the transition of care for patients discharged from intensive care. We are making good progress, but have stumbled upon an unexpected and important observation that we believe needs to be urgently addressed. Patients are being discharged directly from the ICU to the community! Traditionally, discharge from the ICU has been a two-step process; transition to a 'regular' hospital ward for a period of care, rehabilitation and assessment, and then return to the community (e.g., home). However, because of growing demands on our healthcare system, patients are being discharged directly from the ICU to the community. In 2014, 1 in 10 adult ICU patients in Alberta were directly discharged to the community! This new approach offers potential advantages (e.g., could be more efficient) and disadvantage (e.g., might not be as safe), but we don't know because it has not been studied.
Aim: To expand my team's work to re-design the transition of care for patients discharged from intensive care.
Focus: Critically ill patients discharged directly from the ICU to the community.
Jurisdiction: Alberta
Approach: Through the program of research we will develop an evidence-informed 'ICU discharge tool kit' that supports all patients - those who receive care on a hospital ward before leaving hospital and those that return directly to the community. This tool kit will be similar to the World Health Organization's Surgical Safety Checklist, and will be designed to ensure that the right patient is discharged at the right time to the right setting with the right care plan.
Team: Health professionals and interested citizens
Research outputs and more information
- Stelfox, HT et al. 2018. JAMA Intern Med
- Stelfox, HT et al. 2016. Intensive Care Med
-
Dr. Jill Tinmouth, Sunnybrook Research Institute

Project title: Improving colorectal cancer screening in Ontario: An embedded health services research program
Embedded Health System Partner: Cancer Care Ontario
Brief Bio: Dr. Jill Tinmouth is a Gastroenterologist and a Clinical Epidemiologist. She attended New York University School of Medicine (1995) and completed her fellowships in Internal Medicine (1999) and Gastroenterology (2000) at the University of Toronto. Subsequently, she pursued further study in Clinical Epidemiology, receiving her PhD in 2004 from the University of Toronto. She is currently appointed as a Staff Physician at Sunnybrook Health Sciences Center, as Scientist at the Sunnybrook Research Institute Inc., as an Adjunct Scientist at the Institute for Clinical Evaluative Sciences, as an Assistant Professor in the Department of Medicine at the University of Toronto and is cross-appointed to the Department of Health Policy Management and Evaluation. She was appointed as the Lead Scientist for Ontario’s colorectal cancer screening program, ColonCancerCheck (CCC), in May 2011.
At Issue: Colon cancer is an important health problem but fortunately, there is high quality evidence to support screening as a way to prevent CRC and death from CRC. All Canadian provinces have organized colon cancer screening programs; Cancer Care Ontario (CCO) launched the CCC program in 2007. Colon cancer screening is a multistep complex process with many moving parts which is characterized by many transitions in care across the health care system, including between and within the community and hospitals.
Aim: To conduct research that supports and drives the design of the CCC program, addresses identified priority policy initiatives for the program and improves the quality of colonoscopy in the province of Ontario.
Focus: The primary focus of my work is on "care design": the design and implementation of efficient and effective colon cancer screening through formal program, with a focus on improving the quality of colonoscopy.
Jurisdiction: The work will be conducted in the province of Ontario.
Approach: Dr. Tinmouth proposes 3 projects that will include 1) navigation of patients with abnormal colon cancer screening tests; 2) improving cancer screening among First Nations and Métis in Ontario and 3) endoscopist report cards to improve colonoscopy quality. The proposed research objectives are tightly aligned with CCO's priorities and strategic directions; thus, this program of research is well positioned within CCO to produce transformative research that will improve the quality, efficiency and effectiveness of cancer screening in Ontario.
Team: Key stakeholders include Prevention and Cancer Control at CCO, the Aboriginal Cancer Control Unit at CCC and the Ontario Colonoscopy Quality Management Partnership.
Research outputs and more information
- Tobias, et al. 2020. Healthcare Policy
- Ivers N, et al. 2019. Current Oncology
- Llovet D, et al. 2018. American Journal of Gastroenterology
- Leddin D, et al. 2018. Gastroenterology
- Palter VN, et al. 2018. Genetics in Medicine
-
Dr. Ian Zenlea, Trillium Health Partners

Project title: Improving Care Transitions between the Hospital and Community for Youth with Obesity
Embedded Health System Partner: Trillium Health Partners
Brief Bio: Ian Zenlea is a pediatric endocrinologist and medical lead of the KidFit Health and Wellness Clinic at Trillium Health Partners in Mississauga, Ontario. He received his medical degree from the University of Vermont College of Medicine, completed his pediatrics residency at Yale School of Medicine/Yale-New Haven Hospital, and completed a pediatric endodrinology fellowship at Harvard Medical School/Boston Children’s Hospital. He also holds a Master’s of Public Health in Clinical Effectiveness from the Harvard T.H. School of Public Health, and completed a Patient Safety and Quality Fellowship at Harvard Medical School.
At Issue: Youth obesity is one of the most serious public health challenges of the 21st century. A number of tertiary care centres in Canada offer structured pediatric weight management clinics. Although these programs are effective, dropout is substantial, availability is limited, and access to this specialized care is difficult. These programs do not typically employ a patient- and family-centred approach that incorporates family expectations and perspectives about treatment which contributes to high dropout rates. Therefore, novel care models should be designed with patient-and family-centred services that improve care transitions between the community and hospital-based weight management clinics where youth can be supported with longitudinal integrated weight management strategies.
Aim: To identify and address existing gaps along the continuum of care for obese youth, improving access to specialized care and promoting service integration.
Focus: Youth with obesity
Jurisdiction: The proposed research program will take place within the Region of Peel, Ontario. Peel is characterized by socioeconomic and ethnic diversity and as the largest suburban community in Canada presents special challenges for the effective design and delivery of pediatric healthcare services. The knowledge gained from this research program will be generalized to other settings within Canada that integrate hospital-based weight management programs with available community resources.
Approach: Through novel research methods including social network analysis and experience-based co-design, we will describe the current state of the local health system for obese youth, highlight opportunities for collaboration between healthcare providers and community-based organizations such as public schools, public health agencies, and community centres, and co-design with patients and families a future state community care model that improves care transitions for obese youth between a hospital-based weight management clinic and the community. A culminating research project will bring patients, families, healthcare providers, and community-based organization members together in a learning collaborative to further develop this prototype care model.
Team: This research program is supported by members of Trillium Health Partners’ research institute, the Institute for Better Health.
Research outputs and more information
- Hadjiyannakis S, et al. 2019. Lancet Child Adolesc Health
- Morrison KM, et al. 2018. BMC Pediatr
- Green J, et al. 2019. J Patient Exp
- Zenlea IS, et al. 2017. Clin Obes
- Martel S et al 2019. Family and Child Health Initiative (FCHI) 2019 Community Engagement Report
New Investigator Salary Award
The New Investigator Salary Award program is designed to provide outstanding New Investigators the opportunity to develop and demonstrate their independence in initiating and conducting health research through provision of a contribution to their salary. A New Investigator is defined as a researcher who has held a full time research appointment for a period of 0 to 60 months.
CIHR’s Institutes of Health Services and Policy Research (IHSPR) and Population and Public Health (IPPH), through the Roadmap Signature Initiative in CBPHC, provided funding for 13 New Investigator Awards in the area of CBPHC that have a primary focus on innovative models for chronic disease prevention and management in CBPHC and/or improving access to appropriate CBPHC for vulnerable populations. New Investigators receive $60,000 per year for up to 5 years.
New Investigators
-
Dr. Farah Ahmad

Project title: Interactive Technologies for Mental Health in Primary Care
Brief Bio: Dr. Farah Ahmad is a health service researcher with a focus on primary care settings, psychosocial health, vulnerable communities and eHealth innovations. Professor Ahmad says “Fostering equitable access to healthcare through applied research, teaching and service is my philosophy”. She uses mixed-method research designs which range from randomized controlled trials to in-depth interviews, focus groups and concept mapping. She has taught courses in health informatics, eHealth, health promotion, migration and health and research methods.
At Issue: Mental health (MH) conditions and illnesses are a serious burden. In Canada, one in five individuals experiences a MH problem or illness in any given year leading to a direct cost of $51 billion annually (Health Canada 2002; Lim 2008). Moreover, timely detection and access to care remains a challenge despite availability of effective treatments for common MH conditions. This is concerning given that depression will be the biggest health burden in Canada by 2030. With the onset of global economic recession, MH needs are on the rise and especially among vulnerable communities. Yet, system resources are constrained. This calls for innovative and efficient ways to engage patients and clinicians to address socially sensitive MH issues in a timely manner. To this end, user-friendly interactive eHealth technologies in multidisciplinary primary care settings can facilitate risk assessment, patient education, and referral making; empowering patients and clinicians simultaneously.
Focus: Common mental disorders (e.g., depression, generalized anxiety, PTSD, and alcohol abuse)
Jurisdiction: Ontario
Approach: The proposed five-year research will examine the provision of MH care and health outcomes by incorporating multi-language, person-centered, interactive, computer-assisted health-risk assessment (HRA) tools in the waiting-room of primary care settings with multidisciplinary teams (e.g. Community Health Centers, Nurse Practitioner Led clinic, and Family Health Teams). This builds on and integrates completed and ongoing research on access to primary care; mental health/violence; eHealth; and vulnerable communities. Dr. Ahmad envisions expansion of such HRA facilitated models of care by including several MH conditions and specific groups while incorporating mobile technological advances and creating data linkages. The implications range from graduate training to the system level diffusion of effective models of care for timely detection and treatment of mental illnesses while creating capacity to measure MH and identify trends at the population level to inform policies for optimal resource allocation
Team: researchers, clinicians, program managers, policy makers, trainees, and IT industry
Highlights: Dr. Ahmad’s innovative approach has led to her success in obtaining Early Researcher Award from the Ministry of Economic Development and Innovation, and recognition as York Research Leader 2014. Her research on the Interactive Computer-assisted Client Assessment Survey (ICCAS) for mental health has led to several presentations, training of students, and three publications: Canadian Family Physician (in press), BMC Health Services Research (in press), CMAJ Open (in review). Building on the evidence generated by a pilot RCT, she plans to conduct a multi-site trial to test a hybrid intervention using iCCAS and collaborative care for mental health in primary care settings serving vulnerable communities. She has expanded her program of research to include youth mental health on campus and successfully obtained CIHR eHIPP funds for “Students Mental Health: Virtual Support on Campus".
More information:
Dr. Farah Ahmad
How can we improve mental health inequities and access to care for vulnerable communities? -
Dr. Cheryl Barnabe

Project title: Arthritis Care for Indigenous Populations
Brief Bio: Dr. Cheryl Barnabe completed undergraduate studies, medical school and Internal Medicine at the University of Manitoba. She then joined the University of Calgary in 2006 for her rheumatology fellowship and an MSc in Clinical Epidemiology, supported by the UCB-TAS-CRA Post-Graduate Rheumatology Fellowship. She is currently an Associate Professor with the Division of Rheumatology, Department of Medicine, and the Department of Community Health Sciences, University of Calgary.
At Issue: Arthritis is the most common chronic disease in Canada’s Indigenous community, and has negative effects on physical and mental health. Having arthritis impacts on the ability to do basic activities, work and participate in the community. Indigenous patients experiencing arthritis experiences treatment gaps compared to the general population, which contribute to worse disease outcome.
Aim: To propose new ways of delivering healthcare that better serves the Indigenous community.
Focus: Treatment and care for arthritis.
Jurisdiction: At the local level, new models of arthritis care embedded in the primary healthcare setting I have developed are being delivered and evaluated throughout southern Alberta. I am working with the Bone and Joint Health Strategic Clinical Network and the Population, Public and Indigenous Health Strategic Clinical Network to ensure the evaluation of these models can help secure funding for expansion of these new care models throughout the province of Alberta. At the national level, I am Chair of the Optimal Care Committee for the Canadian Rheumatology Association, and will be leading Indigenous health care delivery competency training initiatives for rheumatologists. I also sit as a member of the Royal College of Physicians and Surgeons of Canada Indigenous Health Advisory Committee, informing revisions to current programs to ensure Indigenous health competency training is incorporated into residency training programs and continuing medical education. Thus, the result of my research program will be a rheumatology workforce prepared at a minimum to collaborate better with primary healthcare providers and provide excellent care to Indigenous patients, if not ideally directly delivering care directly in the primary care home.
Approach: I have completed all studies relevant to defining the burden of arthritis in Indigenous populations, and identified existing care gaps. Models of care informed by these results have been developed and implemented in several centers and are undergoing evaluation within the domains of acceptability and effectiveness.
Team: I collaborate with several Indigenous communities and their members, Indigenous organizations, provincial healthcare organizations, and national professional bodies, as well as academic researchers from both primary and specialty care.
Highlights: Funding was secured to allow an enhancement of the model of care at an existing clinic. A post-doctoral fellow in my lab (Dr. A. Loyola-Sanchez) was awarded a Banting Post-Doctoral Scholarship from CIHR to look at the sustainability of a new model of care in a rural First Nations community, critical to the scale-up of the model of care to other communities. The initial model of care is now being delivered directly at 4 different sites (both urban and on-reserve).
-
Dr. Simone Dahrouge

Project title: Optimizing the performance of our Primary Health Care System
Brief Bio: Dr. Dahrouge is the Research Director and Deputy Chair for the Department of Family Medicine (Ottawa, Ontario). She is a researcher with the Bruyère Research Institute (Ottawa, Ontario). She has a PhD in Population Health and a Master’s degree in Epidemiology from the University of Ottawa. Her current research focuses on the organization of primary care health services research and its effect on quality of care. She is the recipient of a CIHR New Investigator Salary Award (2013-2018). Her main interest is in understanding how primary care can be organized to optimize the quality and equity of the care delivered.
At Issue: Primary health care is the care delivered by family doctors, nurses, and other health professionals to individuals and families in a community. A strong primary health care system effectively meets the needs of its population, resulting in healthier communities and lower costs. Canada has invested billions of dollars in an effort to make its primary health care system more accessible, effective, and fair. Despite these investments, the Canadian health care system still has a number of gaps in which certain groups receive below average care.
Aim: The goal of my research program is to produce evidence about what approaches can best help address these current gaps in equitable access to primary care and to inform policy changes.
Focus: Marginalized populations, including individuals with language barriers, mental health, and with social isolation.
Jurisdiction: Many projects in which I am involved are interprovincial and international collaborations; however, my work in these teams is usually focussed on Ontario.
Approach: I am studying the large variability in Ontario's primary health care practice structure to understand what innovations have likely contributed to optimizing care. A large part of my program is focused on implementation work. For example, we are currently working on project that will evaluate whether a lay navigator attached to primary care practices can help individuals make appropriate use of the community health and social services they need. We are targeting all those with access barriers and are especially interested in the experience of Francophones living in minority situations.
Team: I am working closely with regional health planners, primary health care provider, and patients of vulnerable populations to inform the navigator project from inception to dissemination. That group has worked to establish the priorities, select the intervention and is ensuring that the approach is acceptable to all.
Team Members: I am fortunate to work with a team of nationally and internationally renowned researchers (CIHR Team Grant: IMAPCT and HSRF INSPIRE-PHC) and with the provincial leaders of Francophone health (Working Group on Ontario’s Francophone Communities)
Highlights: My program of research is relatively young and much of the output at this point has been in the making of invaluable partnership and securing funding. A list of the currently active grants is shown below.
Year Source PI or CoI* Type Amount 06/2016 – 09/2018 Ontario Strategy for Patient-Oriented Research (SPOR).
Centre For Patient Engagement in Primary CareNPI Government $101,668 12/2016 – 12/2017 Canadian Institutes of Health Research (CIHR)
Pan-Canadian SPOR Network in Primary & Integrated Health Care Innovations
Examiner les innovations pour soutenir les patients défavorisés ayant des besoins de santé communautaires complexes et intégrésCo-PI Granting Council $67,400 04/2016 – 04/2020 Canadian Institutes of Health Research (CIHR) Ontario SPOR– IMPACT Award
Navigation implementation and support to optimize access to appropriate community services for Francophones living in minority situationsNPI Government $749,450 07/2015 – 09/2018 Canadian Institutes of Health Research (CIHR)
Ontario SPOR - IMPACT Award
A Pragmatic Strategy Empowering Paramedics to Assess Low-Risk Trauma Patients with the Canadian C-Spine Rule and Selectively Transport them Without Immobilization (PI: Vaillancourt, C.)CoI Granting Council $1,456,990 07/2015 – 04/2017 Ontario Ministry of Health and Long Term Care
Applied Health Research Question (AHRQ) – Institute for Clinical Evaluative Sciences (ICES)
Nurse Practitioner Practice Pattern in Primary CarePi Government $22,556 03/2015 – 02/2018 Canadian Institutes of Health Research (CIHR)
Open Competition – Operating Grant
Incentives and disincentives for treating depression and anxiety in Ontario Family Health Teams (PI: Ashcroft, R. R.)CoI Granting Council $291,571 07/2013 – 03/2018 Canadian Institutes of Health Research (CIHR) (in partnership with the Australian Primary Health Care Research Institute)
Team Grant: Community-Based Primary Healthcare
Innovative Models Promoting Access and Coverage Team (IMPACT)Co-PI Granting Council $4,938,600 04/2013 – 03/2018 Canadian Institutes of Health Research (CIHR)
Team Grant: Community-Based Primary Healthcare
Canadian Chronic disease Awareness and Management Program (C-CHAMP)PI
Sept, 2015Granting Council $2,496,975 -
Dr. Andrea Gershon

Project title: The Chronic Obstructive Pulmonary Disease (COPD) Health Outcomes Team (COHORT)
Brief Bio: Dr. Gershon is a scientist at the Institute for Clinical Evaluative Sciences and Sunnybrook Research Institute, a respirologist at Sunnybrook Health Sciences Centre, and an associate professor at the University of Toronto. She also leads the Respiratory Health Program at the Institute for Clinical Evaluative Sciences and is the 2013 Physicians Services Foundation Fellow in Translational Research. Her research investigates health outcomes, health services, and drug safety and effectiveness in individuals with chronic respiratory disease, specifically chronic obstructive pulmonary disease (COPD) and asthma.
At Issue: Chronic obstructive pulmonary disease (COPD), also known as emphysema or chronic bronchitis, is the third leading cause of death worldwide. In Canada, it affects an estimated one in four adults aged 35 and older and is the most common cause of chronic disease hospital admission and readmission.
Aim: My goal is substantial and sustainable improvements in care for Canadians with COPD. This, in turn, will improve their health and reduce strain on our already overburdened health care system.
Focus: Canadians with COPD
Approach: Linked population health data sources--including health administrative data, clinical databases and electronic medical records--and innovative analytic techniques will be used to examine the real world experiences of people with COPD.
The four objectives of my research and knowledge translation program are to:
- Create new knowledge that improves clinical care and policy for people with COPD,
- Identify and fill gaps in quality, evidence-based COPD care,
- Ensure research results are translated into improvements in COPD clinical care and policy and ultimately contribute to improved health and a strengthened health care system, and
- Train and mentor the next generation of respiratory disease researchers and knowledge translation specialists.
Team: I work closely with an engaged network of clinicians, decision makers and stakeholders who ensure our results are immediately relevant and applied in improving clinical care and developing health policy.
More information:
Andrea Gershon, MD, M.Sc.
ICES Central, Andrea Gershon
DLSPH, Andrea Gershon -
Dr. Noah Ivers

Project title: Strategies to Improve Quality of Care: Trial of Interventions to Support Long-term Adherence and Decrease cardiovascular events post-myocardial infarction (ISLAND trial); Programmatic approach to determining how Audit and Feedback may be optimized to improve processes of care
Brief Bio: Dr. Noah Ivers is a scientist at Women's College Research Institute and a family physician at Women's College Hospital. He is also an adjunct scientist at the Institute for Clinical Evaluative Studies and an assistant professor in the Department of Family & Community Medicine at the University of Toronto. His research is focused on systematically developing and evaluating initiatives that aim to improve quality in primary care. He incorporates principles from behavioural sciences to design complex interventions and principles from clinical epidemiology and health services research to evaluate them. He focuses on use of data to drive healthcare decisions through initiatives such as audit and feedback for health professionals as well as tailored reminders to patients to enable evidence-based and patient-centred care. Working with health system stakeholders, he strives to implement large-scale implementation interventions with the potential to close evidence-practice gaps and to evaluate these through pragmatic, cluster-randomized trials.
At Issue: ISLAND trial: Patients who have had a heart attack have high rates of repeat cardiac problems and even death. Fortunately, there are medications that help to reduce this risk. In addition, people who have had a heart attack can further reduce their risk by participating in cardiac rehabilitation programs where they exercise and learn about a healthy lifestyle and the importance of taking medications. However, only 30-40% of patients participate in cardiac rehabilitation and by one year only 50% of patients continue to properly take their cardiac medications.
AUDIT AND FEEDBACK: One of the most common findings is persistent evidence-practice gaps. One of the most common quality improvement strategies is known as audit and feedback, that is, assessing the practice of individual health professionals, teams, and/or organizations, and providing this data back in a way that seeks to prompt changes.
Aim: ISLAND trial: To test strategies to increase the proportion of patients who continue to take their medications and who participate in cardiac rehabilitation.
AUDIT AND FEEDBACK: To determine how to implement audit and feedback in a way that maximizes the potential of the intervention to improve quality of care.
Focus: ISLAND trial: Cardiac care centres where patients may undergo angiography.
AUDIT AND FEEDBACK: Provincial health quality organizations responsible for measuring and improving quality of care.
Jurisdiction: Provincial: Ontario – with potential for replication in other jurisdictions.
Approach: ISLAND trial: Patients who have a heart attack are randomized to one of three options: a) usual care, where no reminders are sent; b) a series of postal letters; c) letters plus a series of automated phone calls, with additional lay health worker telephone follow up of patients who have stopped their medications. We will contact patients after one year to determine whether they are still taking all their medications and whether they participated in cardiac rehabilitation. We will also determine health care use including the rates of repeat heart attacks in each group. We will then compare the costs and benefits of each strategy.
AUDIT AND FEEDBACK: Sequential, cluster-randomized trials comparing different ways of designing performance feedback reports delivered to physicians across the province to determine how the impact of such ‘report cards’ may be optimized.
Team: I partner with relevant decision makers and policy makers in all aspects to ensure that the findings can lead to sustainable policies.
Highlights: ISLAND trial: Recruited >2700 patients to multicentre randomized trial. Engaged relevant decision makers at each centre and at level of the province who are awaiting results of the trial to inform policy decision making.
AUDIT AND FEEDBACK: Working with Health Quality Ontario and other provincial organizations to test approaches to optimizing the design of physician ‘report cards’. A 2x2 factorial trial will launch in fall, 2016.
More information:
DFCM: UofT
Google Scholar
ICES
IHPME
Ossu
PubMed
Researchgate
Twitter
WCRI -
Dr. Dawn Kingston

Project title: Program of Research in Perinatal Mental Health
Brief Bio: Dr. Kingston’s research focuses on 1) Identifying and responding to individual and system barriers to perinatal mental healthcare by developing, testing, and translating novel cost- and clinically-effective technology-based approaches to screening, referral, and treatment in primary care; 2) Understanding the mechanisms that underlie the impact of poor perinatal mental health on long-term maternal and child outcomes. Dawn has over $3M dollars in funding as PI supporting this research, including this CIHR New Investigator Award and an Early Career Transition Award through Alberta Centre for Child, Family and Community Research. She loves working with her research team and credits much of the success of the research to its high level skills and fearless approach to innovation.
At Issue: Mental health problems are among the most common perinatal morbidities, with 1 in 4 Canadian pregnant and postpartum women affected. However, over 85% of pregnant and postpartum women do not receive needed mental healthcare. Mental health problems in these vulnerable women are therefore substantially under-diagnosed and under-treated. Furthermore, little is known about how poor maternal mental health affects child development and mental health.
Aim: To improve perinatal mental healthcare in primary and generate knowledge of how maternal mental health affects child development/mental health.
Focus: Screening and treatment decisions in pregnant and postnatal women
Approach: A series of linked studies address the primary aims. The two foundation studies of the Plan are highly-ranked (1st, 4th) CIHR-funded trials that evaluate the clinical- and cost-effectiveness of novel approaches to perinatal mental healthcare in primary care: 1) mental health e-screening in pregnant and postnatal women; and 2) integrated model of e-screening/electronic decision-making algorithm/online therapy in pregnant women.
Team: A multidisciplinary, multi-site research team with provincial, national, and international membership and collaborates with policy-makers and end-users.
-
Dr. Vicki Kristman

Project title: Preventing Work Disability Through Accommodation
Brief Bio: Dr. Vicki Kristman is an Associate Professor in the Department of Health Sciences at Lakehead University, an Associate Scientist at the Institute for Work & Health, and also holds an appointment in the Dalla Lana School of Public Health at the University of Toronto. She is also an editorial board member of the Journal of Occupational Rehabilitation. Kristman earned a master's at Queen’s University and a PhD in public health at the University of Toronto. She held a CIHR post-doctoral fellowship in work disability prevention and epidemiology at the Toronto Western Research Institute, University Health Network. Her research interests include understanding the influence of workplace factors on work disability, specifically the influence of supervisors and workplace accommodation. She focuses mainly on musculoskeletal and brain injuries. She takes an epidemiological approach, specializing in cohort studies, randomized trials and systematic reviews of observational studies.
At Issue: Work disability is becoming a global health problem with the worldwide aging of the working population. Supervisors of injured workers play a key role in preventing prolonged work absences. Providing supervisors with tools to improve their response and ability to accommodate musculoskeletal and other workplace injuries may improve worker health and disability outcomes.
Aim: To prevent work disability through the provision of work accommodation.
Focus: Focus is mainly on musculoskeletal and brain injury; although, mental health issues have recently become very important precursors to work disability and are also included in my work.
Jurisdiction: Workers compensation systems operate provincially in Canada, but I have taken a national and international approach as I believe accommodation to be an important tool across different jurisdictions.
Approach: The program of research will focus on three specific research questions: 1) how can stakeholders identify or develop accommodations for workers trying to return to the labour force? 2) how can workplaces and employers support the use of workplace accommodations? 3) how do we measure and demonstrate the health and economic impacts of workplace accommodation for all stakeholders? We are answering these questions using a variety of research approaches, in addition to the epidemiological approach. By answering these questions we will learn how best to prevent work disability through accommodation.
Team: The team includes a number of national and international researchers, as well as representatives from workers compensation boards, unions, workplace health and safety organizations, labour, and students.
Team Members: Patrick Loisel (U of T), Sheilah Hogg-Johnson (IWH), Monique Gignac (IWH), Kelly Williams-Whitt (Univeristy of Lethbridge), Marc Corbière (UQAM), Karen Harlos (U Winnipeg), William Shaw (Liberty Mutual Research Institute for Safety), Ben Amick (Florida International University), Cecile Boot (EMGO Netherlands)
Highlights: Awarded Early Researcher Award from the Ontario Ministry of Research and Innovation to involve two Master’s students and a post-doctoral fellow in program of research (CBPHC Objective: build inter-disciplinary and inter-professional capacity for the generation, synthesis and application of CBPHC research including training and mentoring of new CBPHC trainees, investigators, and health professional scientists)
Invited to Hopkinton Conference to lead a paper on “Improving research of employer practices to prevent disability” with a focus on workplace factors.
With the Thunder Bay District Public Health Unit, we were awarded a Ministry of Labour grant “Superior Mental Wellness @ Work: Standard to Action Project” through the Occupational Health & Safety Prevention and Innovation Program to assist workplaces in Northern Ontario to meet the Standard for Psychological Safety in the workplace, and to evaluate related training and social marketing measures.
Awarded a grant from the Workers Compensation Board of Manitoba on “Supervisor and worker perspectives on workplace accommodations for mental health disorders” through the Scientific Research Applications competition to understand factors influencing supervisors’ ability to accommodate mental health disorders in the workplace.
-
Dr.Patricia T Li

Project title: Primary care for children: a research program aimed at improving quality of care
Brief Bio: Dr. Li studies the organization and delivery of health services to children, including primary care and care for common childhood illnesses such as asthma. She is currently conducting a study on the quality of primary care for children in Quebec, focusing on the disparities in outcomes among vulnerable children, including those of different socioeconomic status and those with chronic diseases. She is also examining the evidence behind practices for routine well-child visits to primary care providers. Her studies aim at working with knowledge users (the decision makers and administrators of healthcare, as well as practicing clinicians) to influence healthcare policy and the delivery of healthcare to children.
At Issue: Across Canada, primary care reforms have taken place to improve the primary care system. The province of Quebec introduced new ways for family physicians to practice in groups known as family medicine groups (FMGs) or network clinics. At the moment, we know little about the primary care of children in Quebec. Primary care includes visits to a doctor for management and prevention of health problems. When a child receives primary care, they may have improved overall health and fewer visits to the hospital. The benefit of primary care may be greater for children living in poverty or with chronic diseases such as asthma.
Aim: To inform policy and practices around the quality of primary care for children in Canada
Focus: Our work has focused on childhood conditions (asthma, diabetes, children with medical complexity, obesity, sleep) that are a high burden to children and the health system, and for which preventive care can improve outcomes.
Jurisdiction: Quebec
Approach: First, at the organizational level, Dr. Li is studying the impact of primary care reforms on outcomes for all children in Quebec and those who are vulnerable. Provincial databanks containing all visits to doctors and hospitals are being used to understand how many children have a doctor, who they are seeing, and if FMGs or network clinics are providing better care for children. She will see if primary care reform has reduced the large differences in health outcomes between poor and rich children. Second, at the primary care provider level, Dr. Li is examining ways to support the delivery of preventive care by developing and implementing tools for primary care providers, and improving physician knowledge.
Team: Decision-makers, researchers, and end-users (clinicians and parents)
More information:
-
Dr. Joanna Sale

Project title: A mixed-methods approach to reduce the burden of illness due to fracture
Brief Bio: Joanna Sale is a clinical epidemiologist whose current interests are in evidence-to-care gaps in musculoskeletal conditions, medication use, the patient perspective, older adults with multiple chronic diseases and models of behavior change. While her main area of research is in osteoporosis (patients with osteoporotic or fragility fractures), she is also involved in projects related to pain, osteoarthritis, rheumatoid arthritis, diabetes, asthma and Parkinson’s Disease. Dr. Sale holds an appointment in the School of Graduate Studies at the level of Full Member and she co-coordinates the course Introduction to Qualitative Methods for Health Services & Policy Research (HSR1001H) in the Institute of Health Policy, Management and Evaluation at the University of Toronto.
At Issue: A fragility fracture is one that occurs after a slip, trip, or fall from standing height or less (for example, slipping on ice and breaking a wrist). In general, this type of fracture predicts future fractures and is a sign of poor bone health that requires treatment. Treatment, which includes vitamin D, calcium, and often medication, is known to reduce the chance (or risk) of future fractures. However, fracture patients often do not receive or follow recommendations for bone health treatment. There are many possible reasons for this. One reason may be that the concept of fracture risk is new and patients and health care providers are not familiar with the levels of risk. Another reason may be that patients who need bone heath treatment have other conditions that are perceived to be more serious and compete for their attention.
Aim: The proposed work aims to determine how we can encourage individuals to follow treatment recommendations for bone health after they have had a fracture.
Focus: We are focusing on two areas of research in post-fracture management: 1) how patients understand the concept of “moderate risk” and, 2) how patients with comorbidities manage their bone health.
Jurisdiction: Local, regional, and provincial
Approach: We are using multiple methods for the proposed work. We are interviewing patients who present to a local fracture clinic as well as conducting quantitative analyses on a local and provincial database. As well, we carried out a scoping review in 2015 to examine what was known about individuals in Canada who were assessed as being at moderate risk for future fracture.
Team: The team includes decision-makers, researchers, and end-users (clinicians and patients).
Team Members: To date, members of the above projects have included Dorcas Beaton (St. Michael’s Hospital), Earl Bogoch (St. Michael’s Hospital, Monique Gignac (Institute for Work & Health), Gillian Hawker (University of Toronto), Joanne Ho (St. Michael’s Hospital), Ravi Jain (Osteoporosis Canada), Victoria Elliot-Gibson (St. Michael’s Hospital), Larry Funnell (Osteoporosis Canada), Gilles Boire (University of Sherbrooke), Marie-Claude Beaulieu (University of Sherbrooke), David Lightfoot (St. Michael’s Hospital), Kosalan Akilan (summer student, St. Michael’s Hospital), and Kevin Senior (summer student, St. Michael’s Hospital).
More information:
Sale et al. What do we know about individuals who are assessed as being at moderate risk for future fracture in Canada? Health 2015;7(5):1-7.
-
Dr. Hsien-Yeang Seow

Project title: Improving home and community-based palliative care through primary health care innovations
Brief Bio: Hsien Seow is an Associate Professor, Department of Oncology, McMaster University and the Canada Research Chair in Palliative Care, Cancer and Health System Innovation. He has previously held the Cancer Care Ontario Health Services Research Chair and the Canadian Institute of Health Research New Investigator Award. Dr. Seow earned a PhD in Health Policy and Management from the Johns Hopkins School of Public Health and a BSc from Yale University. He is a health services researcher who works to improve quality and the healthcare service delivery of palliative care for cancer patients and other serious, chronic illnesses.
At Issue: Patients who are dying can suffer from many uncontrolled symptoms, such as pain and shortness of breath. In addition, they experience significant psychological and emotional distress. When we do not meet the needs of patients in the final stages of their life, they often go to the emergency department or get admitted to hospital, which is very expensive. Palliative care is defined as care that improves the quality of life of patients who are dying by relieving symptoms and reducing psychological and emotional distress. Policymakers want to shift palliative care from hospitals to the home and community, because research shows community care can be high-quality at a lower cost. But they do not have enough knowledge on how to do this effectively. In addition, there are often many resources in local communities (e.g. family physicians, home care nurses, etc.) that are available to provide palliative care but they are currently not organized in the best way possible.
Aim: To improve patient care and make the health system better for all Canadians facing the end of their lives.
Focus My work is mostly focused on home and community care and on health system innovation
Jurisdiction: In what jurisdiction/s is your work set? This could be national, provincial, regional or local, please be specific] My work has been foused in Ontario and Nationally.
Approach: In order to improve palliative care for the patient in the home, the program of research will involve projects designed to: 1) improve homecare nursing services to avoid unnecessary hospital and emergency department use across multiple provinces in Canada; 2) understand how interprofessional teams of various care providers can work together to improve the quality of patient care in the home for lower costs; and 3) develop ways to measure high-quality palliative care in the home and community.
Team: Clinicians, nurses, policymakers, health services researchers, patients and families, and home care providers.
More information:
Palliative Care and Health System Innovation
Impact of community based, specialist palliative care teams on hospitalisations and emergency department visits late in life and hospital deaths: a pooled analysis -
Dr. Joanie Sims-Gould

Project title: A Community Based Research Program Focused on "Adding Life to Later Years"
Brief Bio: Dr. Joanie Sims-Gould is an Assistant Professor in the Department of Family Practice at UBC. She is a Canadian Institutes of Health Research New Investigator and a Michael Smith Foundation for Health Research Scholar. The research questions that she addresses can be captured within 3 broad themes; 1. Experiences of marginalized frail older adults within the Canadian health care system, their families and those health care practitioners who work with them; 2. Delivery of home/community based health care and the experiences of unregulated workers who provide the bulk of this care; 3. Intersection between older adult health, socio-economic status and the built environment. Joanie is a Knowledge Translation Scientist and Core Research Member at the Centre for Hip Health and Mobility in Vancouver, BC. She is currently a Project Lead for Active Aging BC (ABC), a program delivered in partnership with BC Ministry of Health and community organizations that aims to improve the health, mobility and social connectedness of older adults in British Columbia.
At Issue: In 2011, an estimated 5.0 million Canadians were 65 years of age or older, a number that is expected to double in the next 25 years to reach 10.4 million seniors by 2036. The majority of older adults prefer to stay at home for as long as possible. However, for many, receipt of home care services is the only option that enables them to remain independently and safely in their home. At present, more than 1.4 million Canadians receive publicly funded home care services annually. As the Canadian population ages and with earlier discharges from hospital, the need for home care and associated costs continue to escalate. To 'age in place' older people also require community and built environments that facilitate their health and mobility. As health and function decline with aging, older adults' ability to engage with challenging physical environments (e.g. poor street lighting or long distances to amenities) diminishes. Advancing knowledge in this emerging field is key to planning and developing effective strategies that allow older adults to grow old at home.
Aim: "Adding life to later years" so that older adults can live independently in their homes for as long as possible, and improving the quality and utility of evidence for policy and practice change that will enable older adults to age in place.
Focus: Enhance the health and mobility of older adults across two settings: delivery and receipt of home care services, and the neighborhood built environment.
Jurisdiction: My work is national, provincial and regional in scope and involves a variety of diverse stakeholders.
Approach: Dr. Sims-Gould has a strong commitment to knowledge mobilization and participatory methods, which ensures that the questions and outcomes are relevant and have impact in the community or with individuals. She endeavours to engage stakeholders in a meaningful way, early in the research process, as this ensures relevance and serves as a vehicle to disseminate research outcomes. Dr. Sims-Gould engages a diverse stakeholder group - older adults and their families, organizations (South Vancouver Neighbourhood House, The United Way of the Lower Mainland, West End Seniors Network Society), health authorities (Vancouver Coastal, Fraser Health), policy makers at the municipal (City of Vancouver & City of Surrey) and provincial level (BC Ministry of Health) as well as national organizations (Canadian Home Care Association, Accreditation Canada) to ensure that my research reflects real needs (and questions) and that the findings are ‘brought back’ in a format that is usable.
More information: Joanie Sims-Gould
-
Dr. Isabelle Vedel

Project title: Adapting and improving the quality and effectiveness of primary care services for Alzheimer’s disease
Brief Bio: Dr. Isabelle Vedel is a public-health physician and an assistant professor in the Department of Family Medicine at McGill University. She is also an investigator at the Lady Davis Institute of the Sir Mortimer B. Davis - Jewish General Hospital. She completed a postdoctoral fellowship in research on health services associated with treatment of chronic diseases (health care services organization, health management, and information technology) at McGill in 2012. Dr. Vedel’s main research interests are the organization of health care services and primary health care for older people and for people with multiple chronic diseases. Her research focuses on the health services associated with management of chronic diseases, in particular Alzheimer’s disease and related disorders.
At Issue: Alzheimer’s disease is a major concern for policy makers, clinicians and the public, because of the number of people who have this disease, its consequences for these people and their family caregivers, and the costs involved. To improve the care provided to people with Alzheimer’s disease, Family Medicine Groups in Quebec and Family Health Teams in Ontario and New Brunswick have implemented collaborative primary care models. The implementation dynamics and the impacts of these models will have to be updated before they can be put into general use.
Aim: The objectives of this program are to identify the most effective care models in the scientific literature; to determine the impacts of the models implemented in Ontario, Quebec and New Brunswick, and to analyze the longitudinal process of change within the models implemented.
Focus: People with Alzheimer’s disease
Jurisdictions: Ontario, Quebec and New Brunswick
Approach: Three complementary, synergistic studies will be carried out: 1) a systematic review of the literature; 2) a quasi-experimental longitudinal study comparing sites that have implemented the model with sites that have not, to measure the effects of the models on indicators of quality of care (obtained from patients’ records) and indicators of accessibility and continuity of care, health status, and use of services (obtained from medical/administrative databases); 3) a longitudinal qualitative study of the implementation of the models and the dynamics of change. This research program will have major impacts, including a lasting impact on health programs and notable improvements in primary care for people with Alzheimer’s disease.
Team: A committee of partners from the three provinces as well as other provinces, including patients and caregivers, health ministry policy makers and managers, and clinicians, will be involved throughout this participatory research program.
More information: Isabelle Vedel
-
Professor Fiona Webster

Project title: Finding the complex patient in patient-centred care: an institutional ethnography of chronic pain management in family medicine (COPE)
Brief Bio: Professor Fiona Webster is an Associate Professor who is cross-appointed between the Institute of Health Policy Management and Evaluation (IHPME) of the Dalla Lana School of Public Health (DLSPH) and the Wilson Centre for Medical Education Research. She also holds a status appointment with the Social and Behavioral Sciences Division of DLSPH where she is interim co-lead (2016-17). She currently teaches a graduate course in qualitative research methodologies and methods through IHPME. Her formal training is in sociology and specifically institutional ethnography. Her research interests are in the social organization of care delivery, standpoint theory, and the clinical and policy management of chronic pain that is grounded in the patient experience.
At Issue: Patients with chronic conditions and multiple morbidities represent a growing challenge for health care globally. Improved coordination of care is considered essential for providing more effective and cost-efficient care for these patients with complex needs. Osteoarthritis is one of the most common and debilitating chronic conditions, yet osteoarthritis care is often poorly-coordinated. Primary care is usually the first contact for patients requiring relief from chronic pain. Our previous work suggests discordance between the policy goals of improving patient care and the experience of patients. We plan to investigate the empirical context of the primary care setting by focusing on primary physicians’ conceptualizations and performance of their work in treating complex patients with chronic pain. This will allow for an exploration of how primary health care is – or could be – integrated with other services that play an important role in health. While there has been a great deal of attention paid to identifying the epidemiology of multi-morbidity and patient complexity, comparatively little attention has been paid to the processes of care that treating complex patients entails, and to identifying what high-quality, patient-centered care for these patients should look like in practice.
Aim: We aim to identify the complex patient from the standpoint of primary care health professionals, and to ground our investigation in their accounts of the work that caring for complex patients entails. Drawing on over 45 interviews and ethnographic observations with primary care providers (primarily physicians) in various settings in Ontario, our study interrogates the notion that the most complex patients are older, comorbid adults. While a recent quantitative study (Grant et al, 2011) has examined patient complexity from physicians’ perspectives using a web-based survey tool, ours is the first study that we are aware of that uses qualitative interview methodologies to examine complex patients from the lived experience of primary care providers.
Focus: The focus of our work is on the social organization of care for patients who suffer from chronic pain and other co-morbidities.
Jurisdiction: Our work is set in the province of Ontario and includes the ethnographic study of care in urban, rural and remote Northern communities.
Approach: This study employs the approach of institutional ethnography (IE) to investigate how
Team: We are building a lasting collaboration between physicians, scientists and policymakers that draw upon the strengths of each discipline, and produce significant contributions to the scholarly literature, advances best practice in the management of complex patients in primary care and ultimately improves the care of patients and their families living with chronic, multi-morbidities. The project was originally housed at the Department of Family and Community Medicine (DFCM) at the University of Toronto, the largest Family Medicine training program in North America. The P.I. has moved to the Institute of Health Policy Management and Evaluation (IHPME). Four of the team members are faculty at the DFCM, including one researcher (Dr. Krueger) and three primary care physicians (Dr. Wilson, Dr. Bhattacharyya and Dr. Upshur). Three of the researchers on the team represent the disciplines of psychology (Dr. Katz) and epidemiology (Dr. Davis and Dr. Krueger). In addition to the primary care perspective, we have representation from acute care/surgery (Dr. Yee). While the majority of work is being conducted by Dr. Webster and her research associates and students, these experts are consulted at larger team meetings that will be held at key times in the research process.
Highlights: The COPE study team has published one paper, has submitted another two and is awaiting a decision, and is in the process of submitting another three articles for publications, for a total of six. Through this grant I have been able to offer training to 1 post-doctoral fellow, 1 PhD student from York University (on a practicum), a medical student, a clerk, and several other graduate students. We have also leveraged our funding in order to develop related studies looking at: 1) medical trainees experiences of education for pain management; 2) a scoping review of the history of pain management education and training; 3) a media analysis of 20 years of media reporting on opioid addiction. We have presented our findings at several national and international conferences. At our next team meeting in October 2016 we are focusing on reaching out to decision-makers at the policy and practice levels.
More information: We are in the process of developing a website for this study.
Applied Public Health Chairs
The Applied Public Health Chair program represents a partnership between:
- CIHR’s Institute of Population and Public Health,
- Public Health Agency of Canada (PHAC),
- CIHR-Institutes of Indigenous Peoples’ Health, Aging, Health Services and Policy Research, Musculoskeletal Health and Arthritis, Neurosciences, Mental Health and Addiction, and the HIV/AIDS and STBBI Research Initiative as well as the Alberta Innovates – Health Solutions (AIHS), the Fonds de recherche du Québec – Santé (FRQS).
The program supports innovative population health research that improves health equity for citizens in Canada and around the world. This can be achieved through interdisciplinary collaborations and mentorship of researchers and decision makers in health and other sectors. Through CPBHC, 3 Applied Public Health Chairs were funded.
Applied Public Health Chair – Paula Braitstein
Applied Public Health Chair – Damien Contandriopoulos
Applied Public Health Chair – Wendy V. Norman
Other Researcher profiles

Susan Chatwood
Sharing best practices to improve the health of remote northern communities

Martin Fortin
Improving primary health care for people living with multiple chronic diseases

Amanda Terry
Encouraging the use of electronic medical records among primary health care practitioners
- Date modified: