Rare research: Uncovering the mystery of Batten disease
Neurodegenerative diseases affect millions of people around the world—and while we often associate this type of illness with getting older, that’s not always the case. There are some types that affect children, including a group of disorders collectively known as Batten disease (also called neuronal ceroid lipofuscinosis, or NCL, in medical terms).
Batten disease is a rare, genetic (inherited) disease that affects anywhere from 1 to 35 births for every 500,000 babies born. As with other neurodegenerative diseases, it damages the central nervous system (brain and spinal cord) as the cells in that part of the body stop working properly or die. Children with Batten disease are often born healthy and develop normally until symptoms such as loss of vision, loss of motor skills and seizures set in, usually between the ages of 3 and 13 (but sometimes even before the age of 1 or 2). As the disease progresses, children become blind, unable to walk, talk, or swallow and often remain in a wheelchair or bed.
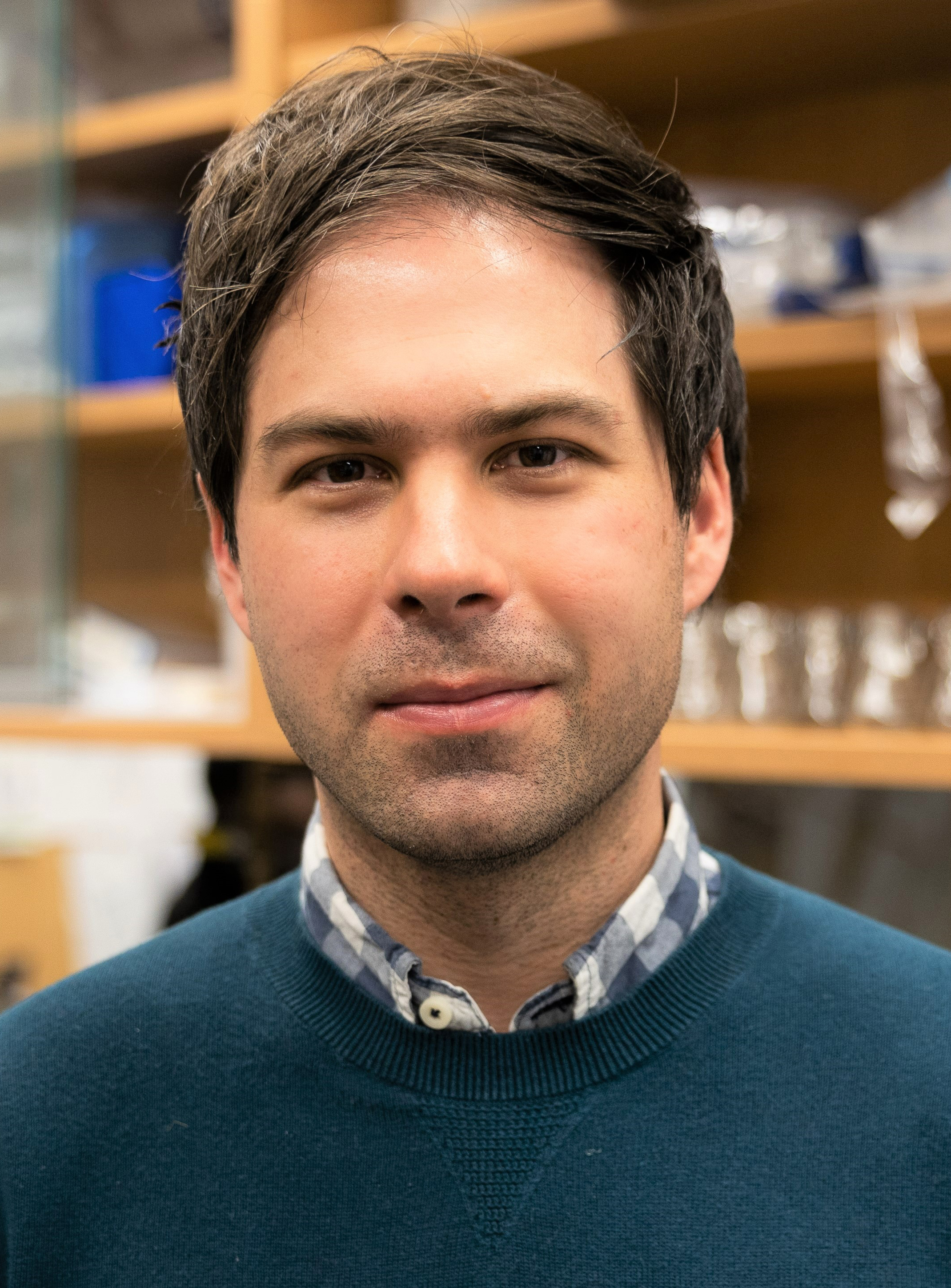
“There’s currently no cure for the disease, and very few treatments,” explains Dr. Robert Huber, an associate professor in the Department of Biology at Trent University who studies the gene mutations associated with Batten disease. “And although life expectancy tends to depend on the age when symptoms develop, it is eventually fatal.”
What makes Batten disease so complex is that it is caused by a mutation in any one of 13 different genes called ceroid lipofuscinosis, neuronal (CLN) genes. Each CLN gene is associated with a different subtype of the disease (CLN1, CLN2, etc.). So, for example, a mutation in the CLN3 gene causes the CLN3 subtype of Batten disease. The subtypes share many of the same symptoms but vary in severity and the age when symptoms first appear.
Dr. Huber and his team are researching the CLN5 subtype of Batten disease. “Historically, CLN5 disease was a relatively understudied subtype of NCL and the cellular role of the CLN5 protein was poorly understood,” Dr. Huber says. “Also, it’s becoming increasingly evident that researching one form of Batten disease can reveal new insight into other subtypes of the disease. So, our work has the potential to inform research on other NCL subtypes.”
The cellular waste management system
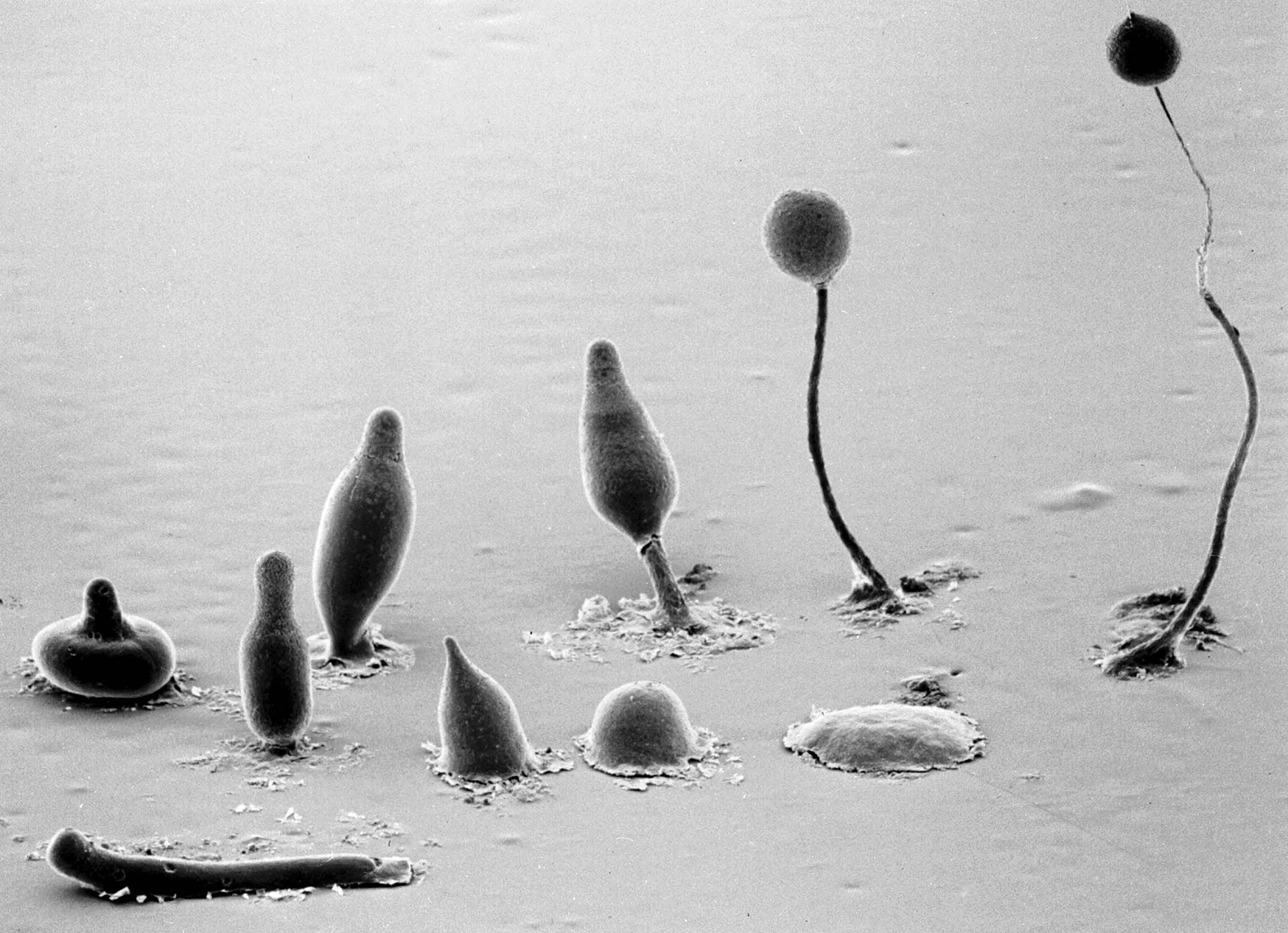
Photocredit: Grimson & Blanton, Texas Tech University
Dr. Huber’s research is focused on understanding how mutations in the CLN5 gene lead to Batten disease.
“What we do know is that the CLN5 gene gives cells instructions on how to make the CLN5 protein, and that protein plays an important role in the breakdown of cellular material,” he explains.
All cells breakdown material and create waste products—it’s just part of the regular process of being a functioning cell—and this means that cells also need to get rid of that waste. If cells can’t efficiently break down material or remove waste, then the material can build up and prevent cells from working properly.
In Batten disease, the cellular waste management system doesn’t function properly. Either material cannot be broken down effectively or waste material cannot be removed from cells. Specifically, the lysosome—a part of a cell that normally acts like a garbage disposal—doesn’t (or can’t) do its job. Over time, the build-up of material interferes with cells so badly that symptoms of the disease start to appear.
“Since the CLN5 protein plays a role in regulating how the lysosome functions, mutations in the CLN5 gene ultimately affect how the cell processes and breaks down material,” Dr. Huber says. “But we still need more research to better understand exactly what is happening and why.”
One way of studying these types of cellular processes is to use a ‘model organism.’ With this type of work, researchers use and even manipulate organisms to study genetic and cellular processes. In Dr. Huber’s case, his lab uses a microbe found in soil called Dictyostelium discoideum, also known as a cellular slime mold.
“This particular organism has been used for almost a century to study and understand a wide range of cellular processes,” Dr. Huber continues. “It’s easy to grow and genetically manipulate and contains many genes that are similar to genes associated with human disease.”
One of those genes happens to be CLN5, which is how Dr. Huber and his team discovered that the CLN5 protein plays an essential role in regulating the function of lysosomes. His team can introduce genetic mutations into the slime mold, and since those mutations mimic those that have been identified in Batten disease patients, Dr. Huber can study how those mutations affect cell behaviour.
The road to targeted therapies
Several years ago, it was reported that the CLN5 protein was not only found inside the cell but also outside. Dr. Huber and his team are investigating this finding further and their work has shown that the CLN5 protein is one of six CLN proteins that get released from cells. Dr. Huber’s research is now geared toward understanding why the CLN5 protein is released, especially since it’s known that the protein is needed inside the cell, and how this process relates back to the disease.
“We think the release of the CLN5 protein from cells is a normal process. However, we want to understand why the protein is being sent outside the cell,” Dr. Huber says. “Does the protein function outside the cell once it’s released? Does this function underlie CLN5 disease? Or does the release of the protein prevent it from carrying out its normal function inside cells within the lysosome? And in that case, can we maybe confine it within the cell or reduce the amount that’s released?”
Answers to these questions, along with finding out the exact role of CLN5 within a cell’s waste management system will hopefully lead to targeted therapies that can correct or minimize the effects of the mutations that cause Batten disease.
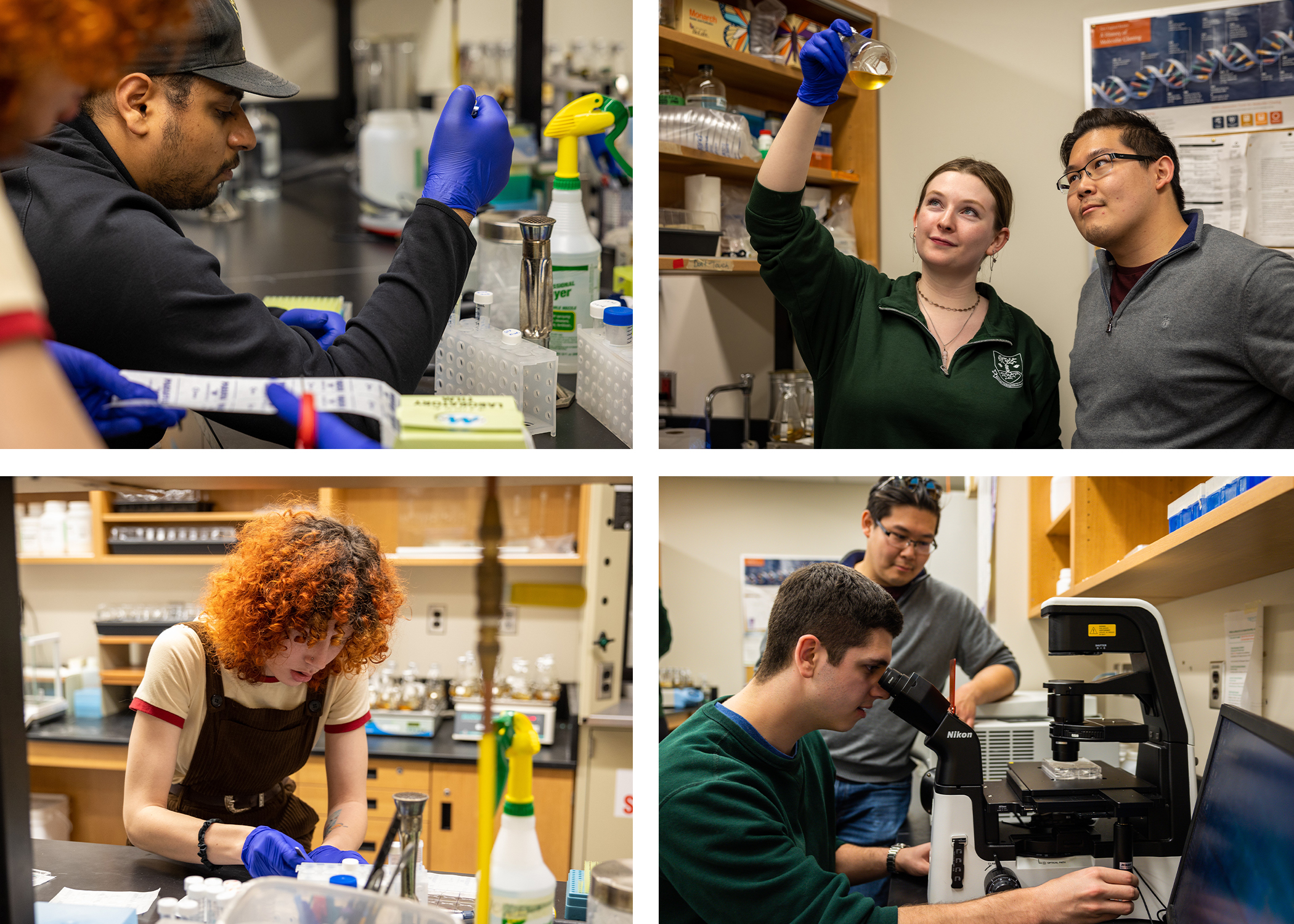
At the same time, Dr. Huber’s team is also testing whether drugs or compounds already approved to treat other diseases could be repurposed for Batten disease. With this line of research, the team deletes the CLN5 gene from the slime mold so that it starts to display abnormal cellular behaviour. “The goal is to then apply one of those drugs or compounds to cells to see if doing so allows the cells to function normally,” Dr. Huber says. “This is an important part of our research. Manipulating the gene allows us to better understand the biology of the CLN5 protein, but then seeing whether the drug or compound can restore normal cell behaviour might be one step towards a treatment.”
Making a difference for families
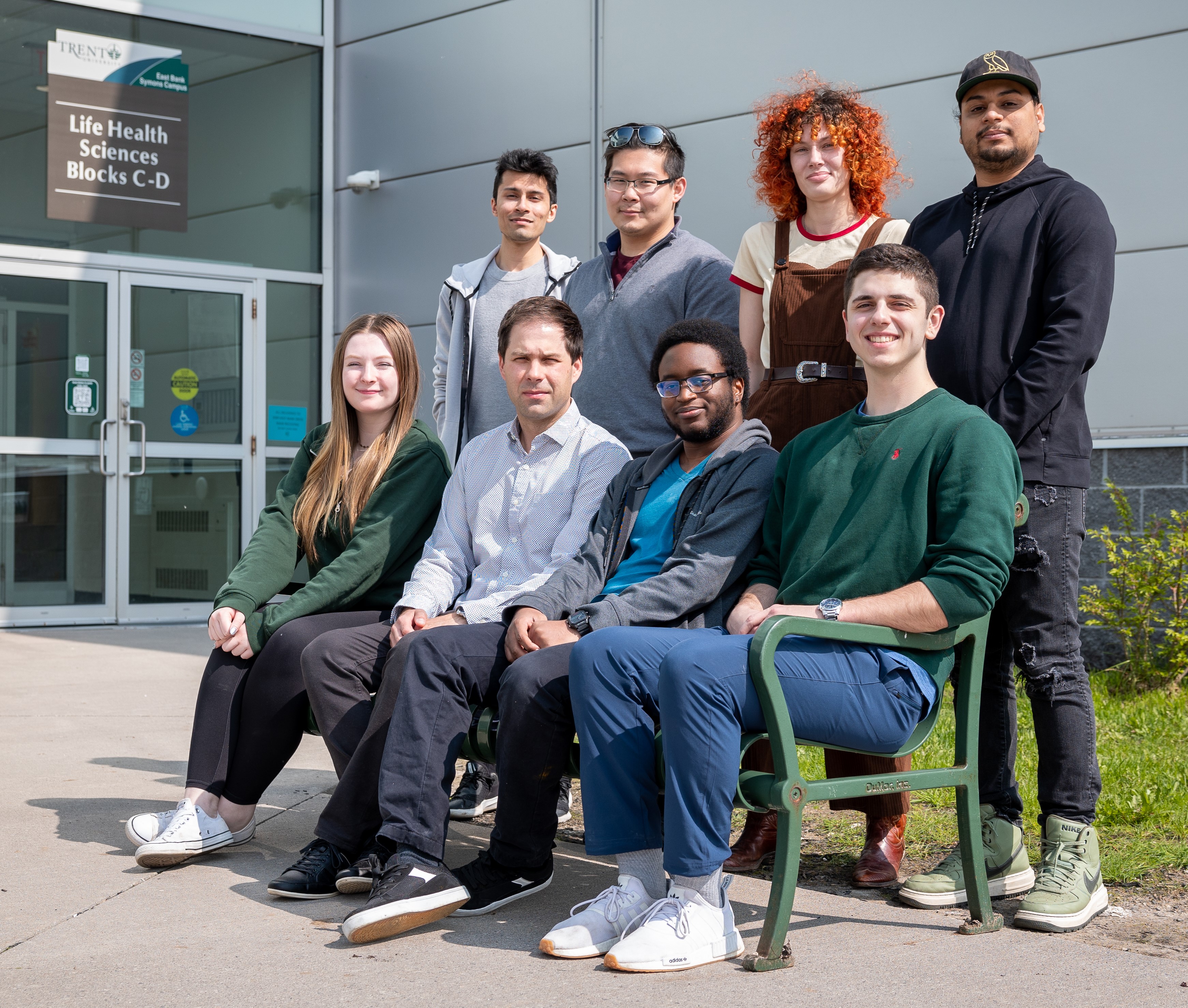
Dr. Huber and his research team are working alongside Dr. Stephane Lefrançois at the Institut national de la recherche scientifique and McGill University. Dr. Lefrançois is taking the same genetic manipulations Dr. Huber is applying in his research and introducing them into human cells.
“Hopefully what we learn from the two systems is similar and then we can combine that information to get a better understanding of what's happening within patient cells,” Dr. Huber says. The next step after that will be taking the lessons learned from the slime mold and human cells and applying them to cells obtained from Batten disease patients. “It starts with fundamental research to enrich our understanding of the CLN5 protein and then we build upon that to bring us closer to answers and treatments.”
Dr. Huber says that he sometimes receives emails from families coping with Batten disease thanking him for his work, even though they know that the research results may not come in time to save their child.
“Receiving emails from families is very motivating, knowing that people are paying attention and value the work we're doing. It also reminds us that our work has the potential to make a difference. The human connection is important and is what motivates us to continue looking for ways to help individuals with Batten disease and their families,” he says. “Also, Batten disease highlights the importance of investing in rare disease research. Caring for a child with Batten disease is a devastating situation for families and we need to continue our efforts in trying to understand what is at the root of the disease.”
- Date modified: