A cross-Canada network of researchers is building an integrated approach to Lyme disease

At a glance
Issue
Lyme disease, transmitted by infected ticks, can have serious and long-lasting effects on human health. While the federal government identified Lyme as a nationally notifiable disease in 2009, much remains unknown about prevention, diagnosis and treatment. With a changing climate, the risk of Lyme disease is increasing.
Research
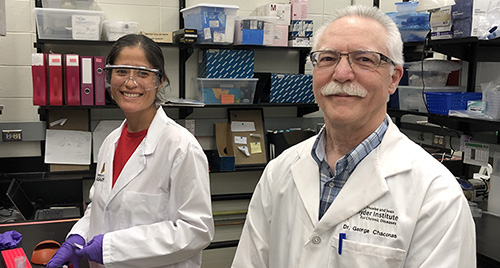
In 2018, with CIHR funding, the Canadian Lyme Disease Research landsNetwork was set up to bring together scientists from various disciplines to study all aspects of this emerging disease. In Calgary, for example, Dr. George Chaconas is studying pathogenesis, while Dr. Manisha Kulkarni is investigating prevention in the Ottawa-Gatineau area. Using a One Health approach that considers multiple disciplines, the researchers engage academics, public health professionals, environmental scientists, health care providers and industry, as well as patients and concerned citizens.
Impact
Using cutting edge imagery, Dr. Chaconas has opened a new way of understanding how the bacterium (Borrelia burgdorferi) “hitchhikes” through the body to cause Lyme disease. For her part, Dr. Kulkarni combines tick surveillance, remote sensing technology and epidemiological data to better understand where ticks are thriving, where people are getting infected, and what can be done to reduce tick density and human exposure. Her research, which is already informing public health policy and urban planning, can integrate climate change models to predict areas of likely risk.
Related stories
The blacklegged tick can be no bigger than a sesame seed, which makes it difficult to spot on human skin. When it grasps its host, it makes no sound. When it bites, it doesn’t sting or make the skin itch. And when it finishes feeding on blood, it falls off the body. If the tick is infected with Borrelia burgdorferi it can transmit the spirochete, or bacterium. Typically, but not always, this leads to a “bullseye” rash. Often, a human may never know they’ve been bitten — unless they start developing symptoms of Lyme disease.
Blacklegged and western blacklegged ticks may carry the spirochete (B. burgdorferi) that causes Lyme disease. These ticks are often found in forests or semi-forested areas, but they also nestle in leaf litter or long grass. In endemic areas, anyone hiking or camping, or even gardening or cutting the lawn, can be at risk of exposure.

Early symptoms of the disease can include fever, chills, fatigue and joint pain. Left untreated, it can lead to serious health issues, including arthritis, cognitive impairment and irregular heartbeat. Five to ten percent of patients who undergo standard antibiotic treatment may continue to experience Lyme-like symptoms, a disorder referred to as Post-Treatment Lyme Disease Syndrome.
Although the federal government identified Lyme as a nationally notifiable disease in 2009, it has been tracking this emerging disease for decades. In 1994, 35 cases were registered across the country. By 2021, the figure had risen to 3,147 for that year, but this is certainly much lower than the actual incidence.
With financial support from CIHR, the Canadian Lyme Disease Research Network was set up in 2018 to build an integrated response to all aspects of Lyme disease. The cross-country network brings together scientists from various disciplines, engaging academics, public health professionals, environmental scientists, health care providers and industry, as well as patients and concerned citizens. Through this One Health approach, they are working to better understand how to prevent, diagnose and treat this emerging disease.
A hitchhiker’s guide to understanding how B. burgdorferi causes Lyme disease
Early in their two-year life cycle, ticks can pick up infections by feeding on small mammals like mice. Later, as they mature, the ticks can transmit this infection to humans, which manifests as Lyme disease. The transmission process is complex and requires at least 1-2 days of tick attachment, making tick removal early after attachment an effective way of preventing Lyme disease.
Dr. George Chaconas, a network scientist at the University of Calgary, is working on two complementary areas of research that could shed light on the development of Lyme disease, and lead to more effective treatments. A professor in the Department of Biochemistry & Molecular Biology and Microbiology, Immunology & Infectious Diseases, Dr. Chaconas previously held the position of Canada Research Chair in Molecular Biology of Lyme Borreliosis from 2003-2017.
“I started working on Lyme disease because, as a protein and DNA biochemist, I found the organism really interesting,” he says. “It’s like a strange visitor from another planet. It has two dozen DNA molecules, which is very unusual for a bacterium. Most of them are linear instead of being circular, and the linear molecules terminate with hairpin ends. How does that happen and how do they function?”
In one area of his work, he studies a major protein that sits on the surface of the bacterium. Initially, antibodies can recognize this protein and clear it from the body, but B. burgdorferi is able to continuously change the sequence of the protein. When that happens, the antibodies can no longer recognize it, a process known as antigenic variation.
“The organism is always one step ahead of the immune system,” says Dr. Chaconas. “If we can understand how that happens and stop it, then the immune system would catch up to the organism and clear it from the body, once and for all.”
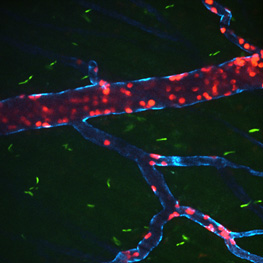
His lab also studies how the spirochete “escapes” from the blood vessels to invade localized tissue, like the knee, the brain or the heart. When an infected tick takes a blood meal from a human, the spirochetes get into the skin and start to multiply. They subsequently enter the blood vessels and then “escape” the circulatory system to invade surrounding tissue.
“They essentially hitchhike all over the body,” says Dr. Chaconas. “They can get out of the blood vessels or disseminate to a huge number of places. If they get out in your knee, you can end up with Lyme arthritis. If they escape blood vessels in the brain, you can have all sorts of neurological problems. If they get into your heart, you can get carditis.”
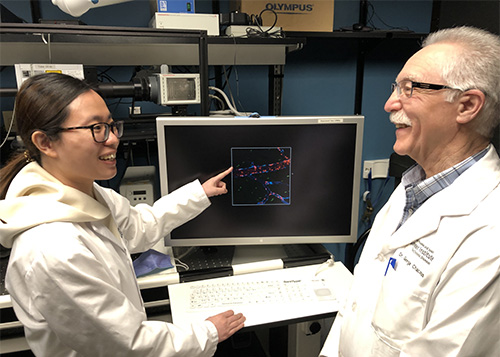
For the past two decades, scientists have made little progress in understanding this process, known as vascular escape. Dr. Chaconas, however, has been able to move research forward by using cutting edge imaging technology pioneered by Dr. Paul Kubes to study the mammalian immune system. Their collaboration, which began around 2008, has led to several joint papers.
“With intravital imaging, we can see these spirochetes in the blood vessels of a living mouse,” says Dr. Chaconas. “In this way, we’ve identified a new approach to understanding the pathway of the disease. Once we know how that works, we can look for effective ways to stop spirochete dissemination and disease development.”
Understanding the social and environmental factors that can lead to Lyme disease

As part of the Canadian Lyme Disease Research Network, Dr. Manisha Kulkarni is part of a pan-Canadian surveillance effort to track the spread of ticks and Lyme disease risk by monitoring sentinel sites across all provinces. An associate professor in the School of Epidemiology & Public Health at the University of Ottawa, Dr. Kulkarni works with her team to identify the social and ecological determinants for Lyme disease infection in the Ottawa-Gatineau area. What environmental factors make the presence of ticks more likely? How do people’s interaction with the environment increase or reduce their risk?
Nymphal ticks, which are about the size of a poppy seed, are both difficult to spot and to remove from the skin. Since 2017, her team has visited several sites in Ottawa each summer to identify where nymphal tick populations are active. They combine their findings with satellite remote sensing data on different climate and environmental variables that affect the presence of ticks. These include different land cover and types of forest, and whether the land provides habitat for mice, other rodents and birds that are part of the infection cycle.
“We combine the field data with the satellite data to get a better picture over a wider area of where ticks might be found. And then, by using these spatial models with epidemiological studies — where infected people live — we can see where the risk of human infection is greatest, right down to the neighbourhood level,” says Dr. Kulkarni.
As part of their work, they also test ticks for signs of infection since not all ticks will transmit Lyme disease. In 2016, for example, they found infection prevalence in ticks was over the 20% recommended threshold. In response, Ottawa Public Health declared the City of Ottawa at risk for Lyme disease for the first time in 2017.
“With our modelling, we can also predict where ticks are likely to be found based on environmental conditions, and then look at future impacts of climate change, and other changing environmental factors,” she says. “We can then monitor trends and inform health care providers if there’s an increasing risk. Early diagnosis and treatment for Lyme disease infection are very important.”
Apart from helping to shape public health policy, Dr. Kulkarni’s research can also inform urban planning. The team looks at the configuration of forested areas and forest patches within neighbourhoods, and recreational trails to see how they influence the incidence of disease in that community. This, in turn, can lead to interventions like using woodchips to keep ticks off maintained trails.
“I think there are a lot of ways we can work at the local level to empower communities,” she says. “We don’t want to deter people from enjoying nature but just to be aware of the risks and to take precautions.”
Protecting yourself against Lyme disease
Here are some ways to prevent exposure to Lyme disease:
- Wear light-coloured clothing (so you can see ticks better).
- Tuck socks into your pants (so any ticks will not crawl inside your pantleg).
- Use bug repellant.
- Wear clothes treated with permethrin (an insecticide known to combat ticks).
- Stay on marked trails and avoid high grass.
- Run potentially exposed clothes through a dryer to kill any ticks.
- Do a “tick check” on your body after potential exposure to ticks.
- Keep grass and vegetation around the home cut short.
- Clean up piles of leaves in your lawn.
- Create a wood chip border to separate your maintained lawn from the wild.
- Wear gloves while gardening.
- Date modified: