Heart Failure Research Network Grant Funding Opportunity
The following figures are related to the Heart Failure Research Funding Opportunity.
Figure 1: Heart Failure – A Multifactorial Condition
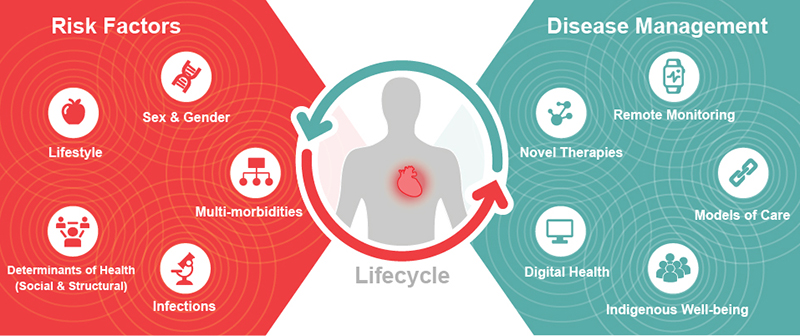
Figure 1 – Long description
Heart failure (HF) is a chronic, progressive and multifactorial condition where the heart is unable to pump enough blood to meet the body's demands for blood and oxygen. The prevalence of heart failure is consistently higher in men than women and occurs across the lifecycle, effecting children, young adults, middle-aged adults and the elderly. A number of risk factors predisposes an individual to heart failure including, but not limited to, determinants of health (social and structural), lifestyle, sex and gender, multi-morbidities and infections. Disease management strategies to address the risk factors for heart failure and/or manage the disease include digital health strategies, novel therapies, remote monitoring, novel models of care, and for Indigenous Peoples; Indigenous-led approaches to well-being. There is an interplay between the disease management approaches and individual risk factors, that when focused on the individual, ultimately determines the most suitable strategies and solutions to improve the prevention, detection, management, and delivery of care of this common condition.
Figure 2: Structure of Network and Application Requirements
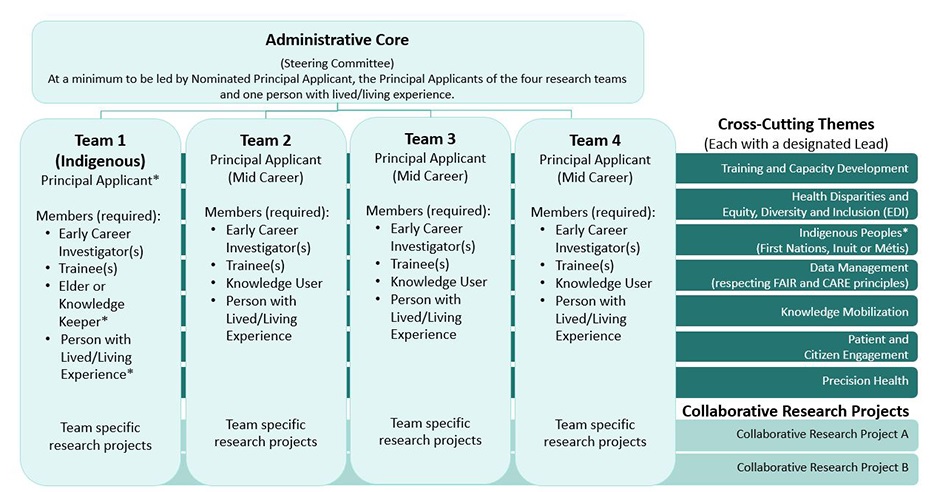
Leadership and membership to reflect EDI, include all four CIHR research pillars and experts from at least four different relevant disciplines
*Self-identify as Indigenous or can provide evidence of meaningful and culturally safe engagement with Indigenous Peoples
Figure 2 – Long description
The Heart Failure Research Network structure is designed to include an Administrative Core (i.e., Steering Committee), a minimum of four (4) Research Teams, and the seven (7) identified Crossing-Cutting Themes outlined in the funding opportunity. The Network Administrative Core (at a minimum) is to be comprised of the Nominated Principal Applicant (NPA), the Principal Applicants (PA) of the four (4) Research Teams and one (1) person with lived/living experience. With the exception of the designated Indigenous Team, each of the other Research Teams are to be led by a PA who is a mid-career researcher and all Teams will be expected to undertake team-specific projects, in addition to engaging and contributing to the required minimum of two (2) Network-wide Collaborative Research Projects. In addition to the PA, each Team will be comprised of a minimum of the following members: Early Career Investigator(s); trainee(s); a Knowledge User; and, a Person with Lived/Living Experience. The Indigenous Team will be led by a PA who self-identifies as Indigenous, or an individual who can provide evidence of meaningful and culturally safe engagement with Indigenous Peoples, and is to include (but not be limited) to the following members: an Indigenous Elder and/or Knowledge Keeper and an Indigenous person with lived/living experience. The seven (7) Network Cross-Cutting Themes, each with a designated Lead, include: Training and Capacity Development; Health Disparities and Equity, Diversity and Inclusion (EDI); Indigenous Peoples (First Nations, Inuit or Métis); Data Management (respecting FAIR and CARE principles); Knowledge Mobilization; Patient and Citizen Engagement; and, Precision Health. The designated Lead for the Indigenous Peoples’ Cross-Cutting Theme must be an individual who self-identifies as Indigenous or can provide evidence of meaningful and culturally safe engagement with Indigenous Peoples. The Network is required to undertake a minimum of two (2) Collaborative Research Projects that engage the Network as a whole. The leadership and membership of the Network are expected to reflect EDI, include all four (4) CIHR research pillars and experts from at least four (4) different relevant disciplines.
- Date modified: